- Visibility 276 Views
- Downloads 28 Downloads
- Permissions
- DOI 10.18231/j.ijmmtd.2020.021
-
CrossMark
- Citation
Clinical characterisation & microbiological profile of otological infections
- Author Details:
-
Diljot Sandhu
-
Veenu Gupta *
-
Deepinder Chhina
-
Manish Munjal
Abstract
Background: Otitis externa & otitis media are notorious ear infections and a major health problem in developing countries causing serious local damage and threatening complications. Early and effective treatment based on the knowledge of causative microorganisms and their antimicrobial sensitivity can ensure prompt clinical recovery and possible complications can thus be avoided.
Aims & Objectives: To identify & characterize the microorganisms causing otological infections & to correlate the findings with the clinical profile of patients.
Materials and Methods: Clinically suspected cases of otological infections were enrolled in the study and the ear discharge was obtained using two separate pre‑sterilized swabs. They were processed for aerobic culture and sensitivity. Drug susceptibility testing was done using Kirby Bauer disc diffusion method.
Results: Among 126 otological cases enrolled, mostly were males. Most affected age group was 51-60 years, Ear discharge, ear pain and feeling of fullness were the commonest presenting symptoms. Clinically 65% were classified into otitis media and 35% into otitis externa. Unsafe Chronic suppurative otitis media was the commonest type. Most common bacterial isolate on culture was Pseudomonas aeruginosa (47.1%). Gram positive bacteria were predominant isolates in otitis externa, while Gram negative bacteria were more common in Otitis media. Antimicrobial profile of Gram negative isolates revealed maximum sensitivity to piperacillin, piperacillin-tazobactum, imipenam and ciprofloxacin. All Gram positive isolates were sensitive to vancomycin, teicoplanin & linezolid.
Conclusion: Continuous and periodic evaluation of microbiological pattern and antibiotic sensitivity of isolates is necessary to decrease the potential risk of complications by early institution of appropriate treatment.
Introduction
Otological (ear) infections mostly encountered in the outpatient department of any medical institution are otitis externa and otitis media.
From the time of its initial description by Mayer in 1844 until World War II, acute otitis externa (AOE) was thought to be a fungal infection. It is a common inflammatory condition usually associated with bacterial and fungal infections of the skin and the subcutaneous tissue of the external ear.[1] Bacteria in otitis externa are S. aureus, Pseudomonas spp. and E.coli. Fungal otitis externa (otomycosis) is mainly caused by Aspergillus niger, A. fumigatus and Candida albicans.[2] It can be a localized AOE or diffuse OE.
Localised AOE (aka ‘furuncle’) is a staphylococcal infection of the hair follicle. It presents with severe pain and tenderness which is out of proportion to the size of furuncle. Movements of the pinna and jaw are painful. Diabetic patients may show recurrent symptoms.
Diffuse OE is inflammation of the meatal skin which may spread to involve the pinna and epidermal layer of tympanic membrane. It is usually caused by trauma to the meatal skin and invasion by pathogenic organisms. It presents with persistent, severe ear pain and ear discharge. Commonly seen in hot and humid climate and in swimmers, because excessive sweating changes the pH of the meatus from acidic to alkaline that favours the growth of pathogens.[2]
Otitis media is an inflammatory disease of the mucosal lining of the middle ear,[3] which can be of various subtypes. These include Acute suppurative otitis media (ASOM), Otitis media externa (OME), chronic suppurative otitis media (CSOM), mastoiditis and cholesteatoma. They are generally described as discrete diseases but in reality there is a great degree of overlap between the different types.
They are classified as acute (ASOM) or chronic (CSOM) depending upon the duration of the symptoms (< 2 weeks or > 2 weeks according to WHO guidelines). It is commonly caused by the buildup of fluid behind the ear drum.
Sources of infection in otitis media are solemnly dependent on the route by which infection reaches the middle ear. Ear infections are mainly bacterial. These bacterial infections of the middle ear normally originate from the upper respiratory tract, with the bacteria entering the ear through the auditory (Eustachian) tube, the principal portal of entry to the ear.[3], [4], [5] Bacterial causes of OM are: aerobes like P. aeruginosa, Proteus spp., E.coli, S.aureus and anaerobes like Bacteroides fragilis and anerobic Streptococci. Most common causes being S. aureus and P.aeruginosa. Other members of Enterobacteriacae might also be involved. Otomycosis (fungal ear infection) can be caused by Aspergillus and Candida spp.[2]
ASOM is commonly characterized by suppuration from the middle ear following perforation of the tympanic membrane. It is the commonest paediatric otorhinological presentation. Otalgia followed by otorrhoea are the commonest symptoms.[2]
CSOM is defined as chronic inflammation of middle ear and mastoid cavity. Incidence of this disease is higher in developing countries especially among lower socio-economic groups. India is one of the countries with high-prevalence where urgent attention is needed. CSOM is an important cause of preventable hearing loss particularly in the developing world and a reason of serious concern, particularly in children.[2], [6] CSOM is usually classified into two types, tubotympanic and attico-antral depending on whether the disease process affects the pars tensa or pars flaccida of the tympanic membrane.[2] Tubotympanic is called as a safe type or benign type as there is no serious complication whereas, attico-antral is called as the unsafe or dangerous type because of associated complications and sequelae may be life threatening. Otological infections are seen in all age groups but are more prevalent in infants and children.[7]
Incidence of these diseases is higher in developing countries especially among low socioeconomic society because of malnutrition, overcrowding, poor hygiene, inadequate health care, and recurrent upper respiratory tract infection. Infection can spread from the middle ear to vital structures leading to complications.[8], [9], [10]
Treatment for otological infections mainly relies on topical antibiotic therapy. Surgeries like tympanoplasty and modified radical mastoidectomy are required in cases with unsafe type of tympanic membrane perforation and complications like mastoiditis respectively.
Aminoglycoside antibiotics were used either systemically or locally but significant side effects especially their ototoxicities have limited its usage. Ciprofloxacin has been increasingly prescribed now. Main advantage of ciprofloxacin is that it is not ototoxic.
Antimicrobial resistance is increasing in common pathogens of otorhinological infections nowadays due to non - judicious use of antibiotics. Resistance mechanism is due to antibiotic deactivating enzymes, alterations in target site of antibiotic and changes in the influx/efflux process. These diseases are now being recognized all over the world because of increased awareness. Therefore, evaluation of microbiological pattern and their antimicrobial sensitivities becomes helpful in prescribing empirical antibiotics for successful and targeted treatment of the infections.
The objective of this study was planned to determine the microbiology of otorhinological infections by identifying all the isolated microorganisms to the species level and to determine the antimicrobial susceptibility profile of bacterial isolates because the susceptibility patterns must be continuously and periodically evaluated to decrease the risk of resistant strains. This also helps to decrease the morbidity and potential risk of complications.
Material and Methods
This prospective study was conducted in the Department of Microbiology, Dayanand Medical College & Hospital, Ludhiana after approval by Institutional Ethical Committee. One hundred twenty six clinically suspected cases of otological infections of any age & either gender were included. Patients detailed demographic, clinical & investigation details were collected.
Ear discharge sample was collected under aseptic precautions on a sterilized swab stick with the aid of aural speculum, prior to instillation of any topical antibiotics. The specimens received in the Department of Microbiology were processed as per standard protocols.
For aerobic culture, the specimen was inoculated by a sterile inoculating loop on Blood agar & MacConkey’s agar and incubated for 24 hours at 37°C. Isolates were identified on the basis of Gram staining, colony characteristics and biochemical reactions. Antibiotic sensitivity testing (AST) was done by Kirby bauer disk diffusion method as per Clinical and laboratory standards institute (CLSI) guidelines. For quality control E.coli ATCC 25922, Pseudomonas aeruginosa ATCC 27853 and Staphylococcus aureus ATCC 25923 were used as per CLSI guidelines.[11]
Clinical characterization
Cases with ear discharge were characterized into otitis externa, acute suppurative otitis media, safe chronic suppurative otitis media and unsafe chronic suppurative otitis media on the basis of duration of disease and clinical presentation.[2]
Data obtained from the study was analyzed by descriptive statistical analysis methods, Frequency distribution, Chi square/Fischer exact test, Significant p value <0.05.
Observations & Results
Among the 126 enrolled cases, the age group of patients ranged from 1 to 85 years. The most affected age group was 51-60 years with 19.9% cases while less than 10% cases were seen at the extremes of age. (Table1[Table 1])
In our study group, 62.7% of the population that presented with otological symptoms were males and 37.3% were females, with a male: female ratio of 1.6:1
| Age group (in years) | No. of patients (%) | Males | Females |
| 0-10 | 9(7.1%) | 6 | 3 |
| 11-20 | 12(9.5%) | 9 | 3 |
| 21-30 | 17(13.5%) | 10 | 7 |
| 31-40 | 21(16.7%) | 12 | 9 |
| 41-50 | 22(17.4%) | 13 | 9 |
| 51-60 | 25(19.9%) | 12 | 13 |
| 61-70 | 8(6.3%) | 7 | 1 |
| 71-80 | 10(7.9%) | 9 | 1 |
| Above 80 | 2(1.6%) | 2 | 0 |
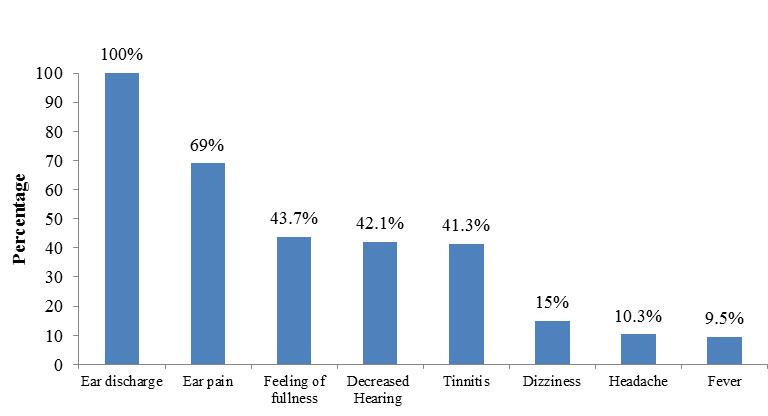
Most common presenting complaint was ear discharge which was seen in all the cases, followed by ear pain in 69%, feeling of fullness in 43.7%, decreased hearing in 42.1% and tinnitus in 41.3%. Dizziness, fever and headache was seen in 10-15% cases. ([Figure 1])
Majority of cases (71.4%) presenting with otological symptoms had long standing complaints ranging from 2 weeks to 10 years.
Unilateral ear involvement was seen in 88% cases (48.4% right ear and 39.6% left ear), while 11.9% had bilateral ears involved.
More than 50% cases had no co-morbidities, while 27% had diabetes mellitus and 20.6% had hypertension.
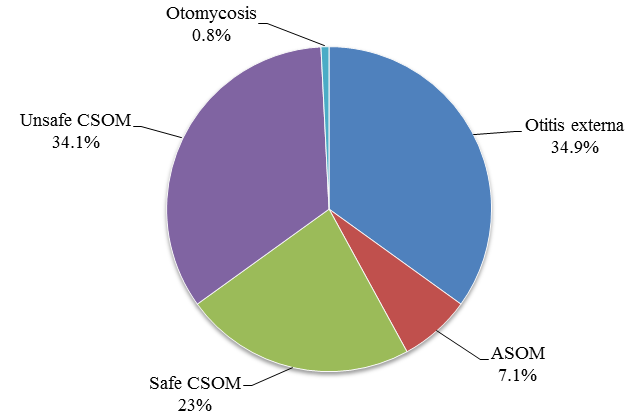
Around 65% cases were classified into otitis media and 35% into otitis externa. The most common type of otological infection was otitis externa and unsafe type of CSOM, followed by safe CSOM. Acute suppurative otitis media was less common. ([Figure 2])
On direct microscopy, Gram positive cocci were seen in 67.5% followed by Gram negative bacilli and Gram negative coccobacilli in 61.9% and 14.3% respectively.
Aerobic culture gave microbial growth in 98 samples, while 28 were sterile. Out of 98 culture positive, 8 had growth of 2 isolates, while 90 had monomicrobial growth, making total of 106 isolates.
Overall Gram staining positivity was 85.7% and culture positivity was 77.8%.
Among the aerobic culture positive samples, 47.1% showed growth of P.aeruginosa, 36.8% S.aureus, followed by 4.7% Klebsiella oxytoca and 2.8% Enterococcus spp. Less number of isolates were obtained for E.coli, Proteus mirabilis, Citrobacter koseri, Proteus vulgaris and A.baumanii. (Table2)
| Clinical presentation | Gram negative isolates (n=63) | Gram positive isolates (n=42) | Fungal isolates (n=1) | |||||||
| P.aeruginosa (n=50) | K. oxytoca (n=5) | C. koseri (n=2) | E.coli (n=2) | P. mirabilis (n=2) | P. vulgaris (n=1) | A.baumanii (n=1) | S.aureus (n=39) | Enterococcus spp. (n=3) | Candida tropicalis (n=1) | |
| Otitis externa (n=29) | 7 | 2 | 0 | 1 | 0 | 0 | 1 | 18 | 0 | 1 |
| Otitis media ( n=76) | 43 | 3 | 2 | 1 | 2 | 1 | 0 | 21 | 3 | 0 |
In otitis externa, Gram positive bacteria were predominant isolates causing infection, while in Otitis Media Gram negative bacteria were more common.

All Gram positive isolates were sensitive to vancomycin, teicoplanin and linezolid. Sensitivity of 73.8% was seen to ciprofloxacin, erythromycin and clindamycin followed by 71.4% to gentamicin. Least sensitivity was seen to penicillin. Three MRSA’s were isolated in our study. (Figure 3)
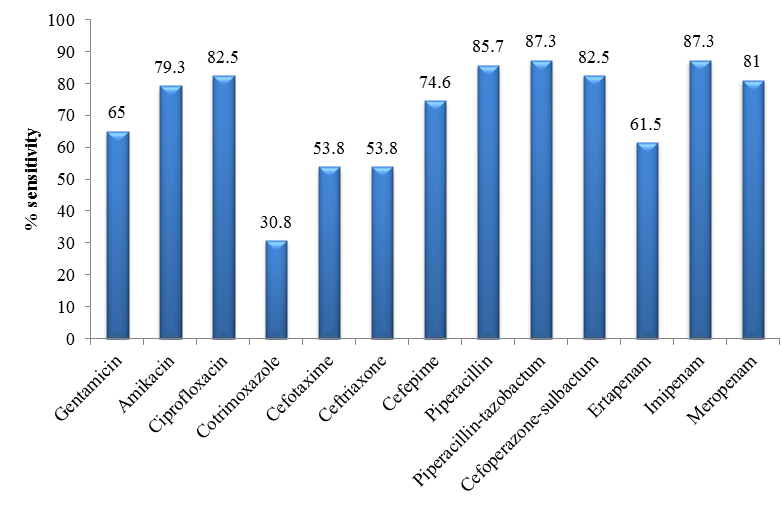
Maximum sensitivity among Gram negative isolates was seen to piperacillin, piperacillin-tazobactum and imipenam (87.3%), followed by 82.5% to ciprofloxacin and cefoperazone-sulbactum and 81% to meropenam, whereas only 30.8% isolates were sensitive to co-trimoxazole.([Figure 4])
In our study, most common complication in patients with ear infections was tympanic membrane perforation (53.2%), followed by hearing loss in (42.1%), mastoiditis in (5.5%), cerebellar abscess in (2.4%) and facial nerve palsy in (1.6%) cases. Only a few cases were observed with mastoid abscess & Citelli’s abscess. Most common type of tympanic membrane perforation encountered was postero-superior type, seen in more than 50% cases followed by central perforation in 28.3% cases and subtotal perforation in 11.9% cases. Attic perforation was observed in only 3% cases. Complications were most common in unsafe type of CSOM with P.aeruginosa as the most common isolate.
Out of 126 patients with otological symptoms, 109 were managed conservatively with oral and topical medication, which mainly comprised of ciprofloxacin, ofloxacin and clindamycin for ambulatory patients and amoxicillin-clavulanic acid and piperacillin-tazobactum among admitted patients. Remaining 17 cases underwent surgery for management of symptoms & complications.
Most common surgical management procedure opted was modified radical mastoidectomy.
Discussion
Ear infections are a commonly encountered entity in routine clinical practice. These infections arise from the external auditory meatus as in otitis externa (OE) or in middle ear causing acute/chronic suppurative otitis media (ASOM/CSOM). Chronic suppurative otitis media is one of the most common chronic diseases of ear and one of the major causes of deafness in India.[12]
In our study group, 126 cases with otological symptoms were included.
There was predominance of otological infections in male patients with a male:female ratio of 1.7:1. This is in accordance with studies done by Arti Agrawal et al.[13] and Shrestha BL et al.[14] This may be a reflection of the overall male predominance of childhood infections due to anatomic, behavioral, and differences in personal habits between males and females.[15] On the contrary, a study from Uttarakhand showed female preponderance with male:female ratio of 1:1.2.[16]
The age group of patients with ear complaints ranged from 1 to 85 years. Overall, the most affected age group was 51-60 years with 19.9% cases, while less than 10% cases were seen at the extremes of age. Otitis externa showed fairly equal occurrence among all age groups, which was similar to the findings of a study done in USA[7] and New Zealand[17] whereas, otitis media was more prevalent among older age groups. Loy et al showed the increased prevalence of otitis media in 30 - 40 years age in his study.[18]
Geographically, our study comprised more of urban patients (68.3%) as compared to patients from rural background (31.7%). This can be due to the fact that our institute is a tertiary care hospital.
Among the most common presenting symptoms, ear discharge was seen in all cases, followed by ear pain (69%), feeling of fullness (43.7%), decreased hearing (42.1%), tinnitus (41.3%) and dizziness (15%).
In our study, overall Gram staining positivity was 85.7% and aerobic culture positivity was 77.8%. Out of 126 cases, microbial growth was seen in 77.8%. Effectiveness of prior empirical antibiotic therapy, poor technique of obtaining ear swabs and sending swabs when diagnosis is uncertain may account for this finding.
Out of 98 culture positive samples, 8.1% had polymicrobial, while 91.8% had monomicrobial growth and this observation was supported by study done by Prakash et al in Uttarakhand and Raakhee T in Andhra Pradesh.[12], [16] In contrast, some researchers found polymicrobial etiology more prominent in otitis media.[19], [20] Difference in results of various authors could have been due to the difference in the patient population studied and geographical variations.
Among the 98 culture positive, the most common aerobic bacterial isolate in our study was P.aeruginosa (49.6%) and S.aureus (37%) followed by Klebsiella oxytoca (4.7%). One case of otomycosis with growth of Candida tropicalis was obtained.
Among the clinical variants, otitis media 81(64.3%) was more common than otitis externa 44(34.9%). Among otitis media, chronic otitis media (88.9%) was more prevalent than acute otitis media (11.1%). High rates of chronic otitis media are attributed to overcrowding and poor hygiene, poor nutrition, passive smoking, high level of nasopharyngeal colonization with pathogenic bacteria and inadequate or unavailable healthcare.[21]
The most common presenting symptom in cases with otitis externa after ear discharge was ear pain (65.9%) and the most common isolate was S.aureus (40.9%) followed by P. aeruginosa (15.9%). This is comparable with the study conducted by Rahul Jayakar et al on cases of acute otitis externa, where 46.5% isolates were P. aeruginosa and 31.9% were S. aureus.[17]
All cases of ASOM presented with ear discharge, followed by ear pain (55.5%), feeling of fullness and hearing loss (44.4%). The bacterial isolates in ASOM cases were S.aureus (50%), P.aeruginosa (40%) and Klebsiella oxytoca (10%). These results are similar to those of a retrospective study done to describe the pattern of distribution and causative bacterial organisms of ASOM from Sokoto, Nigeria, in which otalgia followed by otorrhoea were the commonest symptoms prior to presentation in the hospital. S. aureus (46.2%) was the commonest organism isolated followed by E.coli (23.1%).[22]
All patients with safe CSOM presented with ear discharge followed by complaints of fever (79.3%), feeling of fullness (72.4%), ear pain (68.9%), hearing loss (58.6%). Fewer patients suffered from dizziness & tinnitus. These findings are comparable to those of the WHO report on primary school children from rural Kenya, which reported 63% of ears with CSOM had hearing impairment.(22) The most common bacterial isolates were P.aeruginosa (60.7%) and S.aureus (25%) followed by Klebsiella oxytoca (7.1%). In a study from Bhopal, out of 120 cases of tubo-tympanic type of CSOM, majority were Gram-negative (63.56%). Pseudomonas (37.21%) was the most common bacteria isolated followed by S.aureus (24.81%).[23]
Ear pain, feeling of fullness and hearing loss were the most common symptoms after ear discharge in cases with unsafe CSOM. The most common bacterial isolate was P.aeruginosa (61.1%) and S.aureus (25%) followed by Proteus spp. (8.3%). This can be explained by Pseudomonas being an opportunistic extracellular pathogen that thrives in warm damp external auditory meatus of CSOM patients.[24] These results are consistent with findings of many researchers from all over India.[12], [24] On the contrary, Prakash et al, found Staphylococcus as the most common isolate.[16]
In our study, hearing loss was most profound in patients with CSOM and least in otitis externa. This is comparable with a population prevalence study in Switzerland in 1987 that showed chronic otitis media was the commonest cause of any degree of decreased hearing in 30% of those with hearing impairment.[21]
Antibiotic susceptibility pattern of Gram negative isolates in our study showed maximum sensitivity to piperacillin, piperacillin-tazobactum and imipenam (87.3%), followed by 82.5% to ciprofloxacin and cefoperazone-sulbactum and 81% to meropenam, whereas only 30.8% isolates were sensitive to co-trimoxazole. All Gram positive isolates in our study were sensitive to vancomycin, teicoplanin and linezolid. Sensitivity of 73.8% was seen to ciprofloxacin, erythromycin and clindamycin followed by 71.4% to gentamicin. Least sensitivity was seen to penicillin.
The results are comparable with a study from Bhopal in which P. aeruginosa, had the highest susceptibility to meropenem (97.91%) and S. aureus had maximum susceptibility to vancomycin(100%).[24]
Our results are also consistent with those of a prospective study from Andhra Pradesh done in 2014 on patients of CSOM, according to which ciprofloxacin appeared to be the first line antibiotic (91.52% sensitive) to treat CSOM followed by gentamicin (89.6% sensitive) among the commonly used topical antibiotics.[12]
Previously amoxicillin/ampicillin were used more frequently than quinolones for acute and chronic middle ear infections. But our study has clearly revealed a changing behaviour of micro-organisms showing more sensitivity to quinolones, cephalosporins and gentamycin. So the use of ciprofloxacin has been found superior, both empirically and topically.
Thus it is clear from the present study that bacterial infection is a major etiological factor in otological infections. The sensitivity profile of these bacteria varies a lot and is being affected by drug resistance. Indiscriminate and haphazard use of antibiotics as well as negligence on patient’s part are the factors responsible. As the symptoms subside many patients stop taking antibiotics before the completion of therapy and this allows the partly resistant microbes to flourish. Patients should be instructed to avoid such practice. Therefore, a more rational use of antibiotics is needed to be implied in treatment of patients suffering from a chronically discharging ear to obtain maximal effect.
Conclusion
This study highlights the importance of paranasal mycosis and otological infections in North India. As otorhinological infections are not notifiable infections like many other viral, bacterial or parasitic diseases, hence these are not given much attention and usually diagnosis is established late. Therefore, early diagnosis and recognition of these infections is very important, not only because they are curable in early stages, but also to prevent progression of the disease into the more serious and destructive invasive forms. CSOM like other chronic diseases can limit an individual’s employability and quality-of-life. In many developing countries, including India, prioritizing health-care need is a difficult task. But these days since the awareness among the people is increasing and people are becoming more concerned about the health related issues, there is better recognition of this disease entity. The microbiological assessment is essential to confirm the diagnosis. These microbiological protocols if carried out in well equipped microbiology laboratories having all the advanced facilities available for the isolation and identification of the causative agents, the diagnosis can be simplified since there are no specific clinical and radiological indicators.
Identification of the etiological organisms not only aids in the diagnosis and improves the management of patients, but also assists in advising the patients about the modes of spread, methods of prevention, and anticipating the possible complications. Furthermore, as certain etiological agents are more common in healthcare settings, the healthcare institutions can be directed regarding appropriate hygiene and sterility practice when relevant.
Because of variation in climate, community, patient population and inadvertent use of antibiotics, the pattern of microbiological flora and their resistance pattern to antibiotics varies in otological infections. Continuous and periodic evaluation of the microbial pattern and antibiotic sensitivity of isolates is necessary to decrease the potential risk of complications by early institution of appropriate treatment. In our study on otological infections good sensitivity was seen to piperacillin, piperacillin-tazobactum and ciprofloxacin for Gram negative isolates and linezolid, vancomycin, teicoplanin and ciprofloxacin in Gram positive bacteria.
Therefore, our suggestion to clinicians is that all the patients with otological symptoms should be screened for microbial aetiology. Treatment may require surgical intervention to manage the complications. In refractory cases, systemic antimicrobial therapy may be warranted. The importance of these infections should be recognized and possible preventive and treatment guidelines should be formulated for the patients. We believe that the present study may contribute to an effective management of otological infections.
Source of Funding
None.
Conflict of Interest
None.
References
- Durcan DJ, Goodchild RTS, Wengraf C. Otitis Externa—A Report on a Multicentre Clinical Trial. J Laryngology Otol. 1968;82(4):379-84. [Google Scholar]
- Dhingra PL, Dhingra S. Diseases of ear, nose and throat. . ;2010:54-96. [Google Scholar]
- Brook I, Saantosa G. Microbiology of chronic suppurative otitis media in children in Surabaya, Indonesia. Int J Peditr Otorhnolarygol. 1995;31:23-8. [Google Scholar]
- Daly A. Knowledge and attitude about otitis media risk: implication for prevention. J Pediatr. 1997;3(100):93-6. [Google Scholar]
- Healy GB, DWT. The microbiology of chronic middle ear effusions in children. Laryngoscope. 1977;87(9):1472-8. [Google Scholar]
- Berman S. Otitis media in developing countries. Pediatrics.1995-6;126-31 Berman S. Otitis media in developing countries. Pediatr. 1995;6:126-31. [Google Scholar]
- Roland PS, Stroman DW. Microbiology of Acute Otitis Externa. Laryngoscope. 2002;112(7):1166-77. [Google Scholar]
- Rout M, Mohanty D, Vijaylaxmi Y, Kamalesh B, Chakradhar M. Prevalence of cholesteatoma in chronic suppurative otitis media with central perforation. Indian J Otol. 2012;18(1):7-10. [Google Scholar]
- Morris PS, Leach AJ. Prevention and management of chronic suppurative otitis media in aboriginal children: A practical approach. Community Ear Hear Health. 2007;4:22-5. [Google Scholar]
- Taneja M, Taneja MK. CSOM - A bacteriological study. Indian J Otol. 2009;15:3-7. [Google Scholar]
- . CLSI. M100-S25 Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement. . 2015. [Google Scholar]
- T R, Unguturu S. Bacteriological study of discharging ear in patients attending a tertiary care hospital. Int J Res Med Sci. 2014;2(2):602-60. [Google Scholar]
- Agrawal A, Kumar D, Goyal A, Goyal S, Singh N, Khandelwal G. Microbiological profile and their antimicrobial sensitivity pattern in patients of otitis media with ear discharge. Indian J Otol. 2013;19(1):5-8. [Google Scholar]
- Shrestha B, Amatya R, Shrestha I, Ghosh I. Microbiological Profile of Chronic Supurative Otitis Media. Nepalese J ENT Head Neck Surg. 2012;2(2):6-7. [Google Scholar]
- Falagas ME, Mourtzoukou EG, Vardakas KZ. Sex differences in the incidence and severity of respiratory tract infections. Respir Med. 2007;101(9):1845-63. [Google Scholar]
- Juyal D, Negi V, Pal S, Adekhandi S, Sharma M, Sharma N. Microbiology of chronic suppurative otitis media in a tertiary care setup of Uttarakhand state, India. N Am J Med Sci. 2013;5(4):282-7. [Google Scholar]
- Jayakar R, Sanders J, Jones E. A study of acute otitis externa at Wellington Hospital. AMJ. 2007;7(10):292-9. [Google Scholar]
- Loy AH, Tan AL, Lu PK. Microbiology of chronic suppurative otitis media in Singapore. Singapore Med J. 2002;43:296-9. [Google Scholar]
- Nwokoye NN, Egwari LO, Coker AO, Olubi OO, Ugoji EO, Nwachukwu SC. Predisposing and bacteriological features of otitis media. Afr J Microbiol Res. 2012;6:520-5. [Google Scholar]
- Rao R, Bhaskaran CS. Bacteriology of chronic suppurative otitis media with special reference to anaerobes. Indian J Pathol Microbiol. 1984;27:341-6. [Google Scholar]
- . Report of WHO/CIBA Foundation workshop. Prevention of hearing impairment from chronic otitis media. World Health Organisation. . 1996. [Google Scholar]
- Iseh KR, Adegbite T. Pattern and bacteriology of acute suppurative otitis media. Ann Afr Med. 2004;3(4):164-6. [Google Scholar]
- Thakur P, Poorey V. Clinicomicrobiological evaluation and antibiotic susceptibility in cases of chronic suppurative otitis media. Indian J Otol. 2015;21(2):107-10. [Google Scholar]
- Deb T, Ray D. A study of bacteriological profile of chronic suppurative otitis media in Agartala. Indian J Otolaryngol Head Neck Surg. 2012;64:326-9. [Google Scholar]
How to Cite This Article
Vancouver
Sandhu D, Gupta V, Chhina D, Munjal M. Clinical characterisation & microbiological profile of otological infections [Internet]. IP Int J Med Microbiol Trop Dis. 2020 [cited 2025 Oct 02];6(2):96-102. Available from: https://doi.org/10.18231/j.ijmmtd.2020.021
APA
Sandhu, D., Gupta, V., Chhina, D., Munjal, M. (2020). Clinical characterisation & microbiological profile of otological infections. IP Int J Med Microbiol Trop Dis, 6(2), 96-102. https://doi.org/10.18231/j.ijmmtd.2020.021
MLA
Sandhu, Diljot, Gupta, Veenu, Chhina, Deepinder, Munjal, Manish. "Clinical characterisation & microbiological profile of otological infections." IP Int J Med Microbiol Trop Dis, vol. 6, no. 2, 2020, pp. 96-102. https://doi.org/10.18231/j.ijmmtd.2020.021
Chicago
Sandhu, D., Gupta, V., Chhina, D., Munjal, M.. "Clinical characterisation & microbiological profile of otological infections." IP Int J Med Microbiol Trop Dis 6, no. 2 (2020): 96-102. https://doi.org/10.18231/j.ijmmtd.2020.021
