Introduction
Trichosporon asahii (T. asahii) formerly called T.bigelli is an emerging fungal pathogen seen particularly in immunocompromised patients.
Trichosporon asahii causes white piedra, a superficial infection of hair shafts mainly restricted to tropical regions and less commonly onychomycosis in immunocompetent humans.
In immunodeficient hosts it has been isolated from blood, skin and viscera causing various localized or disseminated deep infections.1
Trichosporonosis has been recognized with increased frequency during the past 10-15 years
Aims & Objective
Identification & Determination of antifungal susceptibility of the yeast Trichosporon asahii.
Case Report
A 65 years male patient k/c/o diabetes and hypertension since 5 years was admitted with the complaints of decreased urine output and burning micturition since 15 days. After the relevant investigations he was clinically diagnosed as Acute kidney injury (AKI) on Chronic kidney disease (CKD).
Empirical treatment was started with antibiotic Monocef
He has undergone dialysis outside our hospital for 4 times before admission and additional 4 dialysis therapy in our hospital.
Complete urine examination (CUE showed many pus cells.
Materials and Methods
Urine sample sent to our laboratory was examined microscopically as wet mount and Inoculated onto Blood agar and SDA plates and incubated overnight at 37oC.
SDA plate was futher incubated for upto 7 days.
The Gram stain of the colonies from both BA and SDA plates were done.
LPCB mount was also done from both BA and SDA plates.
Automated VITEK2 system and MALDI-TOF was done for confirmation of identification.
Antifungal susceptibility done by VITEK2 system.
Repeat two consecutive samples were collected and processed similarly to confirm pathogenicity.
Results
Figure 2
Blood Agar – colonies are tiny, white to cream colored smooth which later on become dry folded.
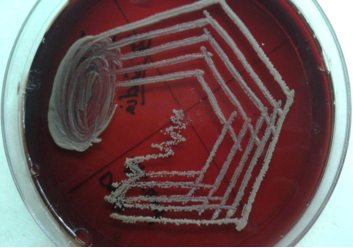
Figure 6
Gram stain (of isolate) -gram positive yeast cells with lateral budding and septate hyphae.

Isolate was confirmed as T. asahii by automated VITEK2 system and MALDI-TOF (matrix assisted laser desorption ionization-time of flight mass spectrometry).
All the three consecutive samples gave similar results which confirmed the pathogenicity
Antifungal susceptibility by VITEK2 system revealed multi resistance to all antifungal drugs tested with preserved susceptibility only to Voriconazole.
Discussion
Trichosporon infections present diagnostic and therapeutic challenges.2 Although Trichosporon is ubiquitous and colonizes many areas, it is a known opportunistic pathogen causing emergent and invasive infections in tertiary care hospitals worldwide.3
Invasive Trichosporonosis is documented mostly in patients with hematological malignancies and other medical conditions associated with immunosuppression.3
Asahii is the predominant causative species and is associated with a poor prognosis
A review of more recent English language literature revealed additional cases of disseminated trichosporonosis among patients with AIDS, malignancy, extensive burns, intravenous catheters, treatment with corticosteroids and heart valve surgery reported from the United states, Europe and Japan.4 Multiple comorbidities such as diabetes and kidney disease may be contributory to the establishment of this infection in our case.
MALDI-TOF appears to be a valuable tool for identifying clinical Trichosporon isolates at the species level.5
Therapeutic management of these infections may also be challenging, since Trichosporon spp. exhibit an intrinsic resistance to the Echinocandins and a poor susceptibility to the Polyenes.6
When assessed by MIC and MFC determinations, Voriconazole is the most active and fluconazole is the least active triazole tested against T. asahii,7 and many other articles are suggestive of Voriconazole as the treatment of choice.
In our case we have advised voriconazole to the patient and the patient showed clinical improvement.
Conclusions
We need to have an increased awareness of disseminated infections due to Trichosporon spp.Such infections require early diagnosis and treatment for fast recovery of the patient.
Due to the natural resistance to echinocandins and polyenes of Trichosporon, breakthrough infections are common.
T. asahii is the predominant causative species and is associated with a poor prognosis, possibly linked to its reduce sensitivity to some azole drugs.
First line therapy should rely on Azole derivatives and particularly Voriconazole, which exhibits the best in vitro activity against Trichosporon sps and significantly leads to a better outcome in patients.6




