- Visibility 169 Views
- Downloads 34 Downloads
- Permissions
- DOI 10.18231/j.ijmmtd.2021.048
-
CrossMark
- Citation
Validation of N95 respirator mask for the Re-use in the pandemic crisis
- Author Details:
-
Nandini M P
-
Prasanna Simha Mohan Rao
-
Prabhu Manohar
-
Naveena J
-
Kavitha K
-
Sathyavathi S *
Abstract
Background & Objectives: The SARS COVID 19 (Severe Acute Respiratory Syndrome Corona Virus Disease 2019) pandemic has created a surge in the need for N95 respirators all across the world. Health care systems are struggling to find a way to cleanse and decontaminate the N95 masks for reuse. To combat the crisis there is a need to validate the N95 mask for efficiency and air filterability on repeated exposure to UV irradiation and vaporized hydrogen peroxide with equal parts of normal saline.
Materials and Methods: To validate N95 respirator mask by using UVGI (Ultra Violet Germicidal Irradiation) method using UV hood and VHP (Vaporized Hydrogen peroxide 6% with equal volume saline 0.9% using an OT fogger machine).
Results: VHP decontamination is the method of choice to repeatedly re-sterilize N95 masks.
Interpretation & Conclusion: Decontamination by the VHP method is more efficient in killing microorganisms within a short duration of exposure (60 minutes). The method retains the texture of the mask material, re-usability and air filterability even with repeated exposure (up to 10 times). UVGI does sterilize the mask but is inferior to VHP in retaining air filterability.
Introduction
There is an increase in the demand for N95 respirator masks all across the entire world, due to the COVID 19 pandemic. Disposable filtering face piece respirators (FFRs) are used very commonly to reduce the exposure to airborne particles. FFRs are the recommended masks for use as part of a comprehensive infection control strategy by the Centre for Disease Control and Prevention (CDC). Manufacturers of respirators [those that are both approved by the National Institute for Occupational Safety and Health (NIOSH) as respirators and approved by the Food and Drug Administration (FDA) for medical uses] recommend that they be discarded if soiled or contaminated. However, the pandemic of COVID -19 has raised serious concern that the manufacturing and supply of FFRs will be unable to meet the sudden increase in demand.[1] Limited reuse has been recommended by some groups and it has also been used widely as an option for the conservation N95 masks during previous outbreaks and pandemics. [1], [2], [3], [4], [5]
But, there are no appropriate decontamination methods that are accepted worldwide. Validation of a decontamination technique is very important and is essential to overcome the current crisis. This study was conducted to validate a method for reuse of the N95 mask. We set out to compare UV germicidal irradiation and vaporized hydrogen peroxide 6% with equal parts of normal saline for their efficacy in killing microorganism and retaining air filterability of the respirator after decontamination.
Objective
To validate the re-use of N95 mask with respect to efficacy of decontamination and air filterability by
UVGI (Ultra Violet Germicidal Irradiation) Method.
VHP (Vaporization Hydrogen peroxide) Method.
Materials and Methods
Seven Silver ShieldTM mask (approved by NIOSH as N95 particulate respirator) for UV validation
Eleven glass petri dish plates for VHP validation
Ten blood agar and MacConkey agar media plates
Peptone broth with bacterial growth.
UV Hood which emits UV in 200nm-300nm range.
Hydrogen peroxide 6% plus equal part of saline 0.9%.
Fogging machine used for fumigation of operation theatres
Incense stick for smoke test & vanilla scented spray.
We used bacterial isolates of Klebsiella species, which are known to be more resistant than SARS COV-2 to various sterilization methods. This would also ensure complete sterilization of the masks before reuse. Direct testing with SARS COV-2 was not possible as we did not have a credited Bio safety Level (BSL3) lab.
UVGI (Ultra Violet Germicidal Irradiation method:
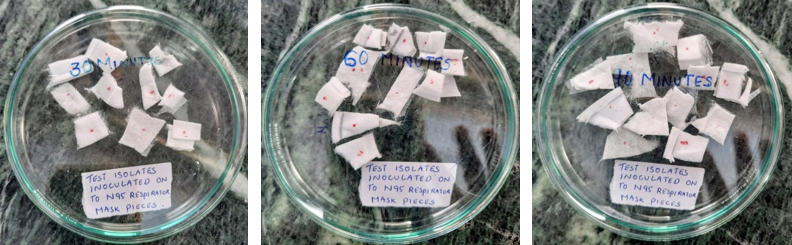
To check the efficiency, one of the N95 mask respirators was cut into several 1cm square pieces. 5 such pieces were inoculated with the test isolate and were put into glass petri plates. ([Figure 1]) One of them was labelled as positive control and was not exposed to UV irradiation. Similarly, other plates were prepared with inoculated mask pieces and were labelled as 5 mins, 10 mins, 15 mins, 20 mins, 25 mins, 30 mins, 60 mins and 90 mins. These were all exposed to UV radiation in the UV chamber for the marked length of time. After exposure to UVGI these pieces were inoculated onto blood agar and MacConkey media and incubated at 37 degree centigrade for 18-24 hours.
Air filtration test was done using smoke and vanilla scented spray after ensuring the N95 mask fit properly to the face by a person who was trained in proper N95 mask donning.
Vaporized Hydrogen peroxide (VHP with equal volume of saline 0 9% method
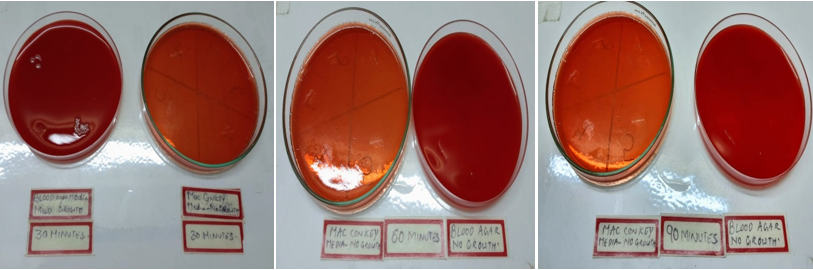
N95 mask pieces (5 per plate X 4 plates = 20 samples) and were labelled 0, 30, 60, 90 minutes were taken in glass petri dishes respectively and were inoculated with the test inoculate. They were exposed to vaporized 6% hydrogen peroxide (VHP) plus equal volume of saline 0.9% for the labelled amount of time using an ultra-low volume operation theatre fogging machine. Later these pieces were inoculated onto blood agar and MacConkey media ([Figure 2]) and respective positive control was incubated at 37 degree centigrade for 18-24 hours.
The N95 masks after exposed to hydrogen peroxide plus equal volume of saline 0.9% were tested for fit and air filterability.
The fit and air filterability tests were repeated daily once the duration of successful kill time was determined using the established safe kill time. The masks were exposed to the successful duration and was tested for fit and air filterability using smoke and vanilla scented spray by a person who was familiar and trained in wearing N95 masks.
Results
We observed 90 percent reduction of bacterial growth in the mask pieces exposed at 45 minutes and total kill at 60 and 90 minutes, with satisfactory positive control on exposure with UVGI.
|
Time |
Blood agar media |
Mac Conkey media |
|
5 minutes |
heavy growth |
heavy growth |
|
10 minutes |
heavy growth |
heavy growth |
|
15 minutes |
heavy growth |
heavy growth |
|
20 minutes |
heavy growth |
heavy growth |
|
25 minutes |
heavy growth |
heavy growth |
|
30 minutes |
mild growth |
mild growth |
|
60 minutes |
no growth |
no growth |
|
90 minutes |
no growth |
no growth |
[Table 2] Air Filterability of the full N95 mask after exposing to UV irradiation at different time frames.
Negative shows inability to smell and taste/Positive shows ability to smell and taste.
Proper fitness of N95 Mask onto face without any gap between mask and face was ensured.
|
Time |
Smoke test |
Vanilla scented spray test |
|
5 minutes |
negative |
negative |
|
10 minutes |
negative |
negative |
|
15 minutes |
negative |
negative |
|
20 minutes |
negative |
negative |
|
25 minutes |
negative |
negative |
|
30 minutes |
negative |
negative |
|
60 minutes |
negative |
negative |
|
90 minutes |
positive |
positive |
Second smoke test and vanilla scented spray test was positive for all samples.
|
Time |
Blood agar media |
Mac Conkey media |
|
30 minutes |
mild growth |
no growth |
|
60 minutes |
no growth |
no growth |
|
90 minutes |
no growth |
no growth |
Repeat fit and air filtration tests were done daily for 10 consecutive days. The tests were all satisfactory for VHP treated masks at an exposure time of 60 minutes, and we stopped at 10th reuse.
Vaporized Hydrogen peroxide exposure was efficient in killing microorganism at an exposure duration of 60 minutes. Aerosol filterability was maintained even after repeated exposure of 10 reuses. UVGI showed microorganism killing efficiency after 60 minutes exposure but can maintain its air filterability only for one exposure
Discussion
There is a worldwide crisis due to the shortage of N95 masks as there is an increase in the demand for N95 masks as a consequence of the SARS COVID19 pandemic. CDC guidelines recommend a combination of various approaches to conserve N95 and other supplies to safeguard health care workers. The CDC recommends that the health institutions implement the reuse or limited reuse of N95 respirators, wherever acceptable.[2] While there are various methods of decontamination of N95 masks in the usage however there is no perfect method for decontamination of N95 masks. But it is important for the decision-makers and users to know the strengths and weaknesses of all the various methods. As there is widespread FFR shortages, it has prompted us to consider the reuse of FFRs during pandemics, whenever there is shortage of the N95 masks and also if it has not been visibly soiled or damaged [4], [6], [7], [8], [9]
FFRs help in removing the pathogenic microorganisms from aerosols which are generated by infected individuals and are thus serve as potential fomites. The viability of influenza virus on inanimate surfaces is well-recognized even though it is highly variable. [10], [11], [12] The previously worn FFRs serve as a reservoir for the spread of virus therefore the reuse of filters exposed to microorganisms requires to be considered carefully. If respirator shortages are to be mitigated through reuse, the use of safe, rapid, cheaper and efficient decontamination methods must be established. [4] CDC implementation recommends that a respirator classified as disposable can be reused by the same worker as long as it remains functional and is used in accordance with local infection control procedures. [1] The HPV method has been found to be potentially safe to be used to decontaminate masks in volumes and this recommendation is also backed by the United States Food and Drug Administration, which has already certified certain vendors to offer hydrogen peroxide vapour treatments.[2]
Hydrogen peroxide and ultraviolet radiation are effective methods of decontamination of medical equipment.[13] We studied to examine the efficacy of decontamination of the mask by both methods. By inoculating the mask with bacterial isolates of Klebsiella species, we endeavoured to ensure complete decontamination of most pathogens including the SARS COV-2 virus. Standard procedure was followed for the decontamination by both methods and also for the incubation for growth of Klebsiella on the culture media. The test can be reproduced and used at other facilities to confirm our results regarding the safe kill times by using both methods. While both the methods showed comparable efficacy in eliminating the pathogen, decontamination by VHP was more better as it showed no growth of the pathogen in MacConkey agar media plates at 30 minutes and conclusive no growth on both media at 60 minutes. The UVGI method showed mild growth of the pathogen in both culture media at 30 minutes and no growth at 60 minutes.
But, it was not known if either method would retain filtration, material strength and airflow integrity of an N95 mask with repeated exposure. We designed a smoke test with incense stick & vanilla scented spray to validate re-use of the decontaminated masks. The air filterability of the mask could be assessed by, whether a trained health care worker donning the decontaminated mask of proper fit could smell or taste the particulate matter on exposure to smoke. The air filterability to particulate matter in smoke can be used to predict the aerosol protective function of the re-used mask. The UVGI method of decontamination caused a significant decrease in air-filterability at the very first cycle of decontamination. The VHP method retained air-filterability for 10 consecutive cycles of decontamination.[14], [15]
Hence the study validates a maximum of 10 times of reuse of the N95 mask after decontamination by vaporized hydrogen peroxide. The whole stock can be exposed to fogging in bulk at the same time. However, it is very imperative and essential to ensure that cross contamination does not occur between the health care workers through interchange of masks. We suggest the masks be marked with initials or colour coded stickers identifying its user. Maintaining a register with the name of the health care worker, date of mask given for decontamination and how many times the N95 mask has come for decontamination cycle is crucial.
Health care workers should be trained for PPE donning and doffing technique, including the N95mask as it is vital to prevent self-exposure to SARS COVID19. Adherence to hand hygiene practice strictly reduces the risk of exposure during doffing the N95 mask. The used masks should be examined for any visible soiling or contamination. The soiled masks lose the ability to protect the wearer due to rough handling or excessive contamination and therefore should be discarded. The hospital administration and Hospital Infection Control Committee (HICC) should be involved in the implementation of N95 mask reuse protocol in the infection control policy.
Health care workers are the critical resources for survival during the current global pandemic. Their occupational safety is of utmost importance to ensure they are able to function in an environment devoid of fear of infection, particularly while facing shortage of personal protective equipment. We hope our study helps in furthering this cause and help our fight against the pandemic.
Conclusion
N95 masks can be effectively decontaminated both by UVGI and VHP methods. However, the VHP method of decontamination is the procedure of choice to re-sterilize N95masks.
Decontamination by VHP is effective at an exposure duration of 60 minute while maintaining air filterability for at least 10 re-sterilization cycles. UVGI was able to sterilize the mask but did not maintain air filterability after single exposure. We recommend 3% vaporised H202 in saline as the method of choice for re-sterilization of N95 masks and have validated it for 10 reuses.
Limitations
We were not able to test using bacteriophages or SARS COV-2 to directly determine direct viral kill ability as we do not have a BSL3 facility.
Acknowledgements
None.
Source of Funding
The authors declare that we have received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The authors declare no potential conflict of interest with respect to research, authorship, and/or publication of this article.
References
- . Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings". . . [Google Scholar]
- Lore M, Heimbuch B, Brown T, Wander J, Hinrichs S. Effectiveness of Three Decontamination Treatments against Influenza Virus Applied to Filtering Facepiece Respirators. Ann Occup Hyg. 2012;56(1):92-101. [Google Scholar]
- Fisher EM, Shaffer RE. A method to determine the available UV-C dose for the decontamination of filtering facepiece respirators. J Appl Microbiol. 2011;110(1):287-95. [Google Scholar] [Crossref]
- Viscusi D, Bergman M, Eimer B, Shaffer R. Evaluation of Five Decontamination Methods for Filtering Facepiece Respirators. Ann Occup Hyg. 2009;53(8):815-27. [Google Scholar]
- Viscusi D. Impact of Three Biological Decontamination Methods on Filtering Facepiece Respirator Fit, Odor, Comfort, and Donning Ease. J Occup Environ Hyg. 2011;8(7):426-36. [Google Scholar] [Crossref]
- Bailar JC, Brosseau LM, Cohen HJ. Reusability of facemasks during an influenza pandemic. Facing the flu. 2006. [Google Scholar]
- Siegel JD, Rhinehart E, Jackson M, Chiarello L. The Healthcare Infection Control Practices Advisory Committee, 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings . . 2007. [Google Scholar]
- Rebmann T, Vassallo A, Holdsworth JE. Availability of personal protective equipment and infection prevention supplies during the first month of the COVID-19 pandemic: A national study by the APIC COVID-19 task force. Am J Infect Control. 2021;49(4):434-7. [Google Scholar] [Crossref]
- Chughtai AA, Seale H, Islam MS, Owais M, Macintyre CR. Policies on the use of respiratory protection for hospital health workers to protect from coronavirus disease (COVID-19). Int J Nurs Stud. 2020;105. [Google Scholar] [Crossref]
- Bean B, Moore BM, Sterner B. Survival of influenza viruses on environmental surfaces. J Infect Dis. 1982;146(1):47-51. [Google Scholar] [Crossref]
- Brady MT, Evans J, Cuartas J. Survival and disinfection of parainfluenza viruses on environmental surfaces. Am J Infect Control. 1990;18(1):18-23. [Google Scholar] [Crossref]
- Boone SA, Gerba CP. Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol. 2007;73(6):1687-96. [Google Scholar] [Crossref]
- Ludwig-Begall LF, Wielick C, Dams L. The use of germicidal ultraviolet light, vaporized hydrogen peroxide and dry heat to decontaminate face masks and filtering respirators contaminated with a SARS-CoV-2 surrogate virus. J Hosp Infect. 2020;106(3):577-84. [Google Scholar] [Crossref]
- Douglas J, Mclean N, Horsley C, Higgins G, Douglas CM, Robertson E. COVID-19: smoke testing of surgical mask and respirators. Occup Med (Lond). 2020;70(8):556-63. [Google Scholar]
- Carr-Locke DL, Soetikno R, Shah S, Kaltenbach T, Shergill A. I Smell Smoke-The Must Know Details About the N95. Am J Gastroenterol. 2020;115(10):1562-5. [Google Scholar]
How to Cite This Article
Vancouver
P NM, Rao PSM, Manohar P, J N, K K, S S. Validation of N95 respirator mask for the Re-use in the pandemic crisis [Internet]. IP Int J Med Microbiol Trop Dis. 2021 [cited 2025 Oct 14];7(4):232-236. Available from: https://doi.org/10.18231/j.ijmmtd.2021.048
APA
P, N. M., Rao, P. S. M., Manohar, P., J, N., K, K., S, S. (2021). Validation of N95 respirator mask for the Re-use in the pandemic crisis. IP Int J Med Microbiol Trop Dis, 7(4), 232-236. https://doi.org/10.18231/j.ijmmtd.2021.048
MLA
P, Nandini M, Rao, Prasanna Simha Mohan, Manohar, Prabhu, J, Naveena, K, Kavitha, S, Sathyavathi. "Validation of N95 respirator mask for the Re-use in the pandemic crisis." IP Int J Med Microbiol Trop Dis, vol. 7, no. 4, 2021, pp. 232-236. https://doi.org/10.18231/j.ijmmtd.2021.048
Chicago
P, N. M., Rao, P. S. M., Manohar, P., J, N., K, K., S, S.. "Validation of N95 respirator mask for the Re-use in the pandemic crisis." IP Int J Med Microbiol Trop Dis 7, no. 4 (2021): 232-236. https://doi.org/10.18231/j.ijmmtd.2021.048
