Introduction
Staphylococcus aureus is a major bacterial human pathogen that causes a spectrum of diseases in humans. Staphylococcus aureus is present in the environment and is also found in normal human flora, located on the skin and mucous membranes (most often the nasal area) of most healthy individuals. S. aureus does not normally cause infection on healthy skin; however, if it is allowed to enter the bloodstream or internal tissues, they cause a variety of serious infections.1 Transmission is normally by direct contact or fomites. It is the leading cause of bacteremia and infective endocarditis,2 which has high mortality and morbidity. It can infect other sites also, which includes osteoarticular, skin and soft tissue, pleuropulmonary, and device-related infections. With the emergence of methicillin-resistant strains, S. aureus related infections have increased significantly and high rates of mortality and morbidity are occurring worldwide.3
Methicillin-resistant Staphylococcus aureus (MRSA) were first reported in the early 1960’s and is now regarded as a major hospital acquired pathogen worldwide. The term methicillin resistant is historically used to explain resistance to any of this class of anti-microbials. It is one of the most common causes of hospital-acquired infection all over the world. Prolonged duration of hospital stay, intravenous drug abuse and irrational use or over-prescription of antibiotics are important risk factors for MRSA acquisition. These factors along with the diversity in mecA gene (responsible for resistant mechanisms of MRSA isolates) pose a major challenge to prevent the spread of disease in both community and hospitals.4
Despite extensive infection control efforts, methicillin resistance among isolates of S. aureus has steadily increased around the world and in India. The major reservoirs of Staphylococcus in hospitals are colonized/ infected in-patients and colonized hospital workers. Transient hand carriage of the organism by healthcare workers account for the major factor for patient to patient transmission. Constant monitoring of these strains is essential in order to control their spread in the hospital setting and spread to the community. It is very essential to know the prevalence of MRSA in any location, because of the public health importance and the threat posed by MRSA infection.5 In North India study, out of 250 Staphylococcus aureus isolated, 115 (46%) were MRSA isolated.6 Similar high rate of prevalence is been noted in other parts of the country.7
Even though the drugs for the treatment of these multidrug resistant pathogens are available, they are costly and toxic. So, to combat this drug resistant pathogen, close monitoring of the resistance pattern of MRSA is essential. Therefore, this study is undertaken to observe any change in the sensitivity pattern of MRSA isolated from patients in a tertiary care hospital over a period of six years.
Aims and Objectives
To analyse and study the change in sensitivity pattern of methicillin-resistant S.aureus over a period of last six years (2013-2018) from a tertiary care teaching hospital. This study determines the prevalence and antimicrobial susceptibility pattern of MRSA in the hospital.
Materials and Methods
Process of collection
This was a retrospective study, carried out in the department of clinical Microbiology of the tertiary care teaching hospital. The antibiotic sensitivity pattern of the MRSA isolated from various clinical samples from January 2013- December 2018 was studied. The sensitivity pattern for the following antibiotic was collected from the database: Gentamicin (10µg), Ciprofloxacin (5µg), Erythromycin (15µg), Clindamycin (2µg), Cotrimoxazole (1.25/23.75µg), Tetracycline (30µg) Vancomycin (30µg), Linezolid (30µg), Teicoplanin (30µg) according to CLSI guidelines.8 The standard ATCC strain of Escherichia coli 25922 and Staphylococcus aureus 25923 were used for quality control of the antibiotic discs. The data collected was entered in the Microsoft excel 2007, coded and were analyzed by frequency and percentage.
Results
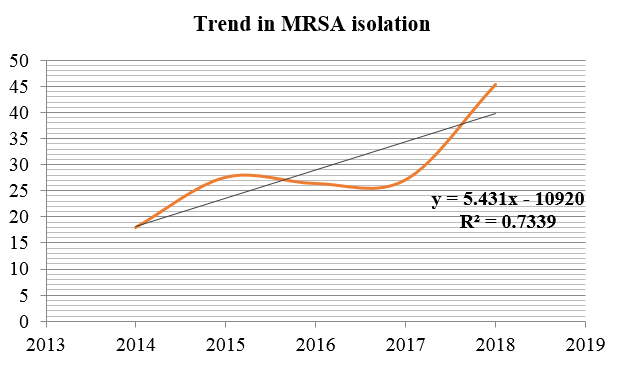
During the study period from January 2013 to December 2018, a total of 3668 patients were registered in the hospital with Staphylococcus aureus infection. Of these, 1006 (27.42%) individuals were found to have MRSA infection. Among the patients infected with MRSA, 52.78% were male patients and 47.21% were female patients showing a slightly higher incidence of the infection in males than females (Table 1). The geriatric patients, i.e., ≥61 years constituted for around 32% infected patients and the least was noticed among individuals <18 years, i.e., 9%. The samples that were received during this period included pus (64.59%), blood (26.23%), urine (5.53%) and sputum (3.65%). The ward-wise distribution of the positive samples showed considerable variation, the highest being OP (65.6%), then IP (26.93%) and finally from the ICU (7.45%). Out of the 75 samples collected from ICU, 41(54.67%) were from MICU. Maximum isolation was obtained during April-June (29.12%) and the least during October-December (19.58%). Throughout the period of study there was a steady rise in the MRSA from 8.77% in 2013 to 45.44% in 2018 (Figure 1). Among the MRSA isolates, there was a steady rise in resistance to Clindamycin and Erythromycin (Fig 2).
Figure 2
Showing trend of resistance rate of various drugs tested against MRSA during the study period.
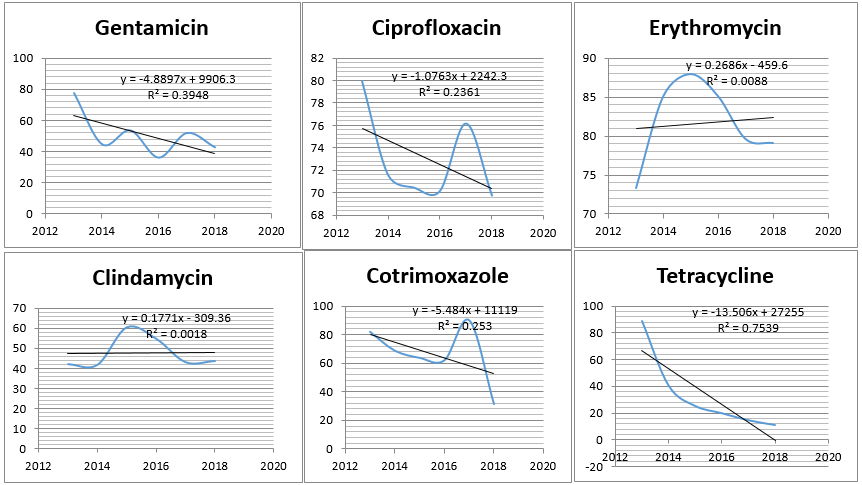
Table 1
Demographic details of the sample analysed during the study period 2013-18.
Antibiotic resistance pattern
In this study, the prevalence and antibiotic susceptibility patterns of various MRSA isolates were obtained from 2013 to 2018. Throughout the period of study there was a steady rise in the MRSA from 8.77% in 2013 to 45.44% in 2018.Among the isolates of MRSA, there was a steady rise in resistance to Clindamycin and Erythromycin as shown in the figure below. All other antibiotics i.e., Gentamicin, Ciprofloxacin, Cotrimoxazole and Tetracycline showed decreasing trend in its resistance pattern (Figure 2). No MRSA strains were found resistant to Vancomycin, Teicoplanin and Linezolid during the study.
Discussion
The six year long study shows an overall MRSA incidence rate of 27.43% in the hospital. The findings are comparable with most of the reports where it ranged between 20% to 32.8%. 9, 10 In the present study, MRSA was mostly isolated from pus and wound swabs whereas a high prevalence of MRSA (35% in ward and 43% in ICU) was observed from blood culture specimens in a study in Delhi. 11 In studies conducted in various hospitals in Nepal, MRSA were mostly isolated from pus specimen compared to other clinical specimens.12, 13 In this study, MRSA isolation rates from ICU (7.45%) and wards (34.38%) were lower than that seen among outpatients (65.6%) which is contrary to another study conducted in India which showed higher MRSA isolation from IPDs (69.82%) than from OPDs (30.18%). 14
We found the occurrence of MRSA to be higher in the geriatric age group i.e., ≥61 years constituted for around 32% infected patients and the least was noticed among individuals <18 years, i.e., only 9%.In a similar study, patients between 0-10 age group showed the maximum MRSA (31.5%), followed by age group 11-20 (26.3%).15 The study showed slightly higher incidence of MRSA infection in males than in females. A similar study conducted in another Indian hospital had slightly higher incidence of female patients than males.14 We have seen downward trend in resistance among most of the antimicrobials except for Erythromycin and Clindamycin. We observed similar increase in resistance to Erythromycin and Clindamycin in MRSA in blood samples from 2012-16.16 A seven year retrospective study showed a reduction in the percentage of resistance in Staphylococcus aureus for the antibiotics Gentamicin and Cotrimoxazole but increase in the drug resistance was observed for antibiotics Amikacin, Ciprofloxacin, Erythromycin and Clindamycin,17 which is contrary to our study. This shows that resistance pattern can vary among different population in different area and warrants the regular monitoring of the changing trends of the resistance pattern among MRSA.
Summary
The study recommends continuous monitoring of antibiotic sensitivity of MRSA, since the drug resistance pattern varies for different antibiotics during the study period. Even though, most of the antibiotics, except Erythromycin and Clindamycin, showed an overall decreasing trend in the antibiotic resistance pattern “between” 2013-18, there were rise and fall of resistance rate in individual antibiotics yearly. Therefore, continuous monitoring of antibiotic sensitivity and rationalizing the use of antibiotics remain an important and effective strategy to minimize the emergence of multi-drug resistant MRSA strains. However, we found no strains resistant to Vancomycin, Linezolid and Teicoplanin, indicating need for prudent use of these drugs for treatment of MRSA related infections.
Conclusion
In the present study, it was observed that there was a steady rise in the MRSA from 8.77% in 2013 to 45.44% in 2018. Among the patients infected with MRSA, slightly higher incidence was noted in males and in the geriatric age group. Most of the MRSA were isolated from pus and exudates (70.57%) from skin and soft tissue infections. Majority of patients samples who were infected with MRSA were from OP (65.6%) compared to IP and ICU admissions. The drug resistance pattern varied for different antibiotics, with an overall decreasing trend in the antibiotic resistance pattern “between” 2013-18. However, there were rise and fall of resistance rate for individual antibiotics annually. But, Erythromycin and Clindamycin showed increasing resistance to MRSA.