Introduction
Increased usage of antibiotics has occurred in the last few decades. As a result, there isan increase in antibiotic resistance among gram-negative bacteria due to the genetic modifications and mutations that lead to multi-drug resistant (MDR) bacteria. The degree of drug resistance in a bacterial species is directly proportional to the use of a particular antibiotic in the community.1, 2 This in turn is associated with increased mortality and morbidity.3 In today’s world it is becoming a critical global issue and the World Health Organisation (WHO) predicts that by 2050 antibiotic-resistant microbes may have caused the death of ten million people every year.4, 5 This is a serious threat because it will impair the medical interventions in terms of managing the patient. 5 Thus, the medical world has taken recourse to Colistin and polymixins as a last resort to fight this menace with some success.
Colistin is a cyclic hexapeptide with a tripeptide side chain acylated at the N terminal by a fatty acid which is of two types: Colistin A (Polymyxin E1) and Colistin B (Polymyxin E2). These two drugs react with the cell membrane of Gram negative bacteria by disturbing the calcium and magnesium ion channels6 Both are very potent and are considered as good antibiotics against Multi Drug Resistant gram-negative Bacteria.7, 8 The effectiveness of colistin against bacterial resistant nosocomial infections caused by Pseudomonas and Acinetobacter spp. has been reported earlier6 However due to the increased usage of colisitn in the last couple of decades has resulted in the development of antimicrobial resistance especially in gram-negative bacteria.6 On the other hand, there is little research happening towards the discovery of new antibacterial and this has a major implication towards treating microbial diseases which is throwing the medical world into confusion.9
The frequent mutations which happens in the genetic material of the bacteria are the primary reasons for the antimicrobial resistance developed in bacteria. Most of the strains of Escherichia coli, Klebsiella pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa are found to have different mechanisms of resistance. 2, 7
The mechanism by which the gram-negative bacteria can develop resistance against colisitn is by mcrgene. It is one such important gene which is present in the bacteria. This gene is rapidly transferred to other bacteria by plasmid mediation leading to the spread of the multidrug-resistant bacteria into the animal and human populations, with resistant bacteria causing major health hazards and almost all bacterial strains have developed this resistance. There are also other mechanisms by which the resistance is attained such as a reduction in the number of receptors on the outer membrane or in the efflux pumps, extended spectrum β lactamases (ESBL), and carbapenemases.10 This has greatly challenged the use of colistin at a global level.
There is also evidence worldwide that reveals the spread of the mcr-1 gene by plasmid transfer to different species and strains of Enterobacteriaceae, including MDR strains.11 Previous reports have shown that the phenotypic and genotypic detection of colistin-resistant E. coli from patients in tertiary care hospital. 12, 13 In addition to this, in Greece, there is an increase of carbapenemases among Enterobacteriaceae to more than 30%.14
There is also detection of colistin-resistant gram-negative bacteria in food, water and animal sources. 14 This indicates the prevalence of colistin-resistant bacteria. Due to antimicrobial resistance, the treatment options for infections caused by multidrug-resistant Gram-negative bacterial strains are limited. This makes it hard to control the possibilities of controlling and treating the spread of hospital contamination. 15
Multiple studies dealt with the prevalence and implications of colistin-resistant gram-negative bacteria in India. 16, 17 However, there are not many studies on the scenario in South India and on which bacterial species in dominant. In this study, we reported the colistin microbial susceptibility against various gram-negative bacterial spp. from clinical isolates in Telangana.
Methods and Materials
Sample collection
This cross-sectional study was ethically approved (SVSMC/IEC-Approval NO-05/2018-625) conducted in intensive care units including PICU, NICU, OBGY, TBCD and other wards of SVS Medical College and Hospital, Mahabubnagar, Telangana during August 2018 to December 2020.This study was carried out on 1852-gram negative bacilli isolated from the bacterial samples obtained from different patients (ICUs). The isolates were collected from clinical microbiology laboratory of our tertiary hospital, all of which were detected Colistin resistance by the MIC studies.
Inclusion criteria
Patients of all age groups (including pediatrics) were included. All the bacterial isolates of Enterobacteriaceae (e.g., Escherichia coli, Enterobacter spp), Pseudomonas aeruginosa were included.
Exclusion criteria
Intrinsically colistin resistant organism including Proteus sps, Providencia spp., Serratia spp and Morganella morgani were excluded.
Bacterial isolates
A total of 1852 consecutive Gram-negative isolates were tested for Colistin susceptibility. All colistin-resistant isolates were processed to detect the Minimum inhibitory concentration (MIC) of antibiotics by the broth micro-dilution method. Interpretation was performed according to the EUCAST breakpoints (www.eucast.org).
Minimum inhibitory concentration (MIC) of colistin
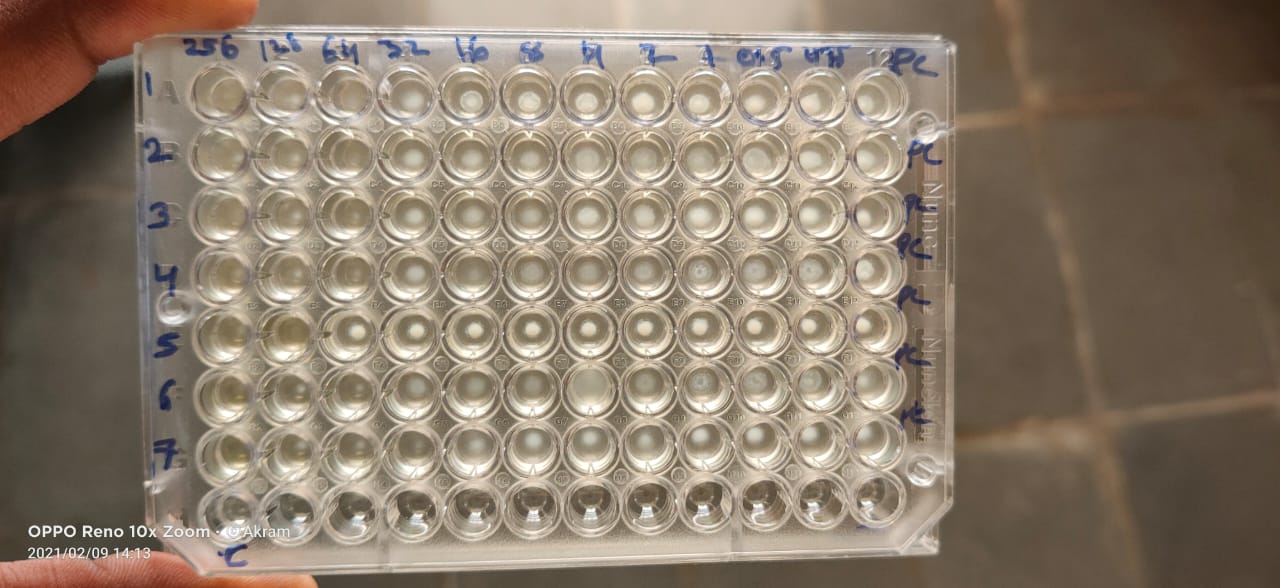
Broth microdilution is considered the reference standard for Polymyxin susceptibility testing. Standard E. coli strain was used as negative control. For the preparation of the antibiotic stock solution, the Colistin drug was obtained in powder form (commercial source with given potency) and stored at 40 C until use. Antibiotic stock solution was prepared based on the requirements.
Inoculum was prepared by making a direct broth suspension of isolated colonies selected from the 24-hour agar plate (blood agar) and adjusting the suspension to achieve a turbidity equivalent to a 0.5 McFarland turbidity standard.
Broth microdilution was done in 96-well microtitre plates, filled with Mueller Hinton II broth (CAMHB, Himedia labs). Serial two fold diluted concentrations of antimicrobial agents and McFarland standard-tested bacteria were added. The plates were incubated at 350C for 24-48 hrs. After incubation bacteria growth was assessed by observing turbidity.
Statistical analysis
Statistical analysis was done using GRAPH PAD PRISM software Ver 6.0 and the data were analyzed by Mean ± Standard Deviation. The relation between two variables was done by Karl Pearson's/Spearmen's correlation test for continuous data and the association between two variables was done by Chi-Square test/Fisher's exact test for categorical data. A P- value less than 0.05 was considered significant.
Results
In the study with Pseudomonas, the p values of susceptibility ranged in most cases between 0.001 to 0.052 showing significant results in the comparison among other antibacterial drugs and Colistin. The colistin is more sensitive to Pseudomonas spp. compared to antibiotics such as PIT, CFS, CPM, IPM, MRP, AK, GEN, CIP, TGC, TRS and DRP (Table 1). In this study, the occurrence of resistance odds ratio of Pseudomonas with carbapenems like DRP and IPM in the presence of colistin is 4.7, 2.9 times more. The presence of colistin with aminoglycosides also shows an odds ratio of more than 3.5. Colistin with cephalosporines (CFS, CPM, CAZ)are 2.2,2.4,2.4 showing that multiple resistance is high. The odds of Pseudomonas 2.6 showing that multiple resistance (colistin and ciprofloxacin) is 2.6 times more. In Pseudomonas, the least odds ratio colistin with Tigecycline is 0.008 which signifies that colistin and tigecycline were both broad-spectrum antibiotics and tigecycline had a good susceptibility.
In the study with E. coli, the p values of susceptibility were significantly more than 0.052 thus showing better results in the comparison among other antibacterial drugs and Colistin. The colsitin is p<0.001 significantly sensitive to E. coli species compared to other antibiotics such as CTR, IPM, TGC and NIT (Table 2). The odds of E. coliare 76.06 showing that multiple resistance for colistin and TGC is 76.0 times more. In E. coli colistin with carbapenems (IPM&MRP) showed an odds ratio of 13.2, and 20.7 respectively. The lowest odds ratio was seen colistin with CTR, CPM, NA, CIP, AK (0.2,0.6,0.3,0.6,0.7).
In the study with Enterobacter spp., the colistinbacterial isolate susceptibility was very less in comparison with other antibacterial drugs and it is resistant against Enterobacter spp. Among the tested clinical isolates, antibiotics such as PIT, CFS, CPM, IPM, MRP, AK, GEN, CIP, CAZ and DRP were less effective against Enterobacterspp (Table 3). In Enterobacter the highest odds ratio was GN and NIT 3.8 and 2.0. The least odds ratio in Enterobactersps is cephalosporines like CFS, CPM with 0.3 and 0.4.
Table 1
Susceptibility analysis of Pseudomonas spp. to colistin and other antibiotics
Table 2
Susceptibility analysis of E. coli spp to colistin and other antibiotics
Table 3
Susceptibility analysis of Enterobacters pp. to colistin and other antibiotics
Discussion
In the modern past, Antibiotic resistance (AR) has concerned the attention in the clinical field worldwide due to growing health-care costs, morbidity, and mortality due to infectious diseases. The condition is worse in developing countries as evidenced by antibiotic susceptibility reports of bacterial isolates. Although drug resistance is primarily a medical concern, the aspects that impact the spread of resistance are environmental, epidemiological, cultural, communal, andcommercial. In most developing and developed countries antibiotic resistance has become a lesser priority when compared with many other infectious diseases. 18
This precarious scenario has led to the use of good old forms of antibacterials such as Colistin and polymixin B, which have shown some promise in combating these diseases. There fore colistin was supposed to be the ‘last-line’ therapeutic drug against multidrug-resistant Gram-negative pathogens in the 21st century. 19 Colistin has been an important antimicrobial agent against aggressive chronic and nosocomial infections due to multidrug-resistant bacteria, and the clinical need for plasmid-mediated colistin resistance in Enterobacteriaceae medically required its use. 20 With the increasing antibiotic resistance, the post-antibiotic era will be more dreadful than COVID-19 pandemic. Colistin resistance is also emerging, which should be detected by every laboratory so as to slow down the speed. 21 In this study deals with the comparison of the susceptibility of Colistin and other common antibiotics on various gram-negative bacterial species isolated from various clinical samples such as blood, pus, urine, and pleural fluid. The prevalence of pathogens and the antibiotic susceptibility testing reports in this study are in consistent with other studies. Some of the antimicrobial resistance patterns and percentages are universal, while others appear to be unique for specific parts of the geographic region. Colistin in this new generation is a potent antibiotic therapy for life-threatening infections. Since this infection spreads world highly resistant organisms pressure the growing importance of antimicrobial therapy. This study was conducted to determine the present susceptibility profile of different gram-negative bacteria in clinical isolates of Telangana.
Similarly, there are other studies in India of the same nature which also obtained the same results. Mathur et al analyzed 802 isolates of K. pneumonia against colistin, and they found that almost 4% were colisitin-resistant.16 Likewise, Garg et al also analyzed the resistance in different bacterial isolates against colistin and found that 9% exhibited carbapenem resistance. These results are consistent with our findings of colistin resistance in Pseudomonas and E. coli spp. 22
In this study only in Pseudomonas and E. coli spp., thus showed good results upon treatment with other antibacterial drugs and colistin in the comparison among other species especially in BAL, pleural and E.T. These results indicate that most of the bacteria studied indicate they must have developed some degree of resistance, which might have mcrgenetic mechanism to colistin, the treatment strategy should be designed judiciously to get better cure. This report can throw some light on the way bacteria are behaving towards colistinin other rare clinical samples of this region and further study is warranted to encompass more species of bacteria. The Pseudomonas and E. coli species, which indicated more susceptibility also must be studied to understand their genetic structure via mcr gene activity.
Conclusion
This study showed the prevalence of better susceptibility of Colistin against gram-negative bacilli such as Pseudomonas and E. coli spp. In Telangana state and this can give a better cure for nosocomial infections caused in various hospital wards. The other bacteria studied could have developed genetic modification in the form of mcr gene mutation. However a greater number of studies are required to quantify the data upon colistin sensitivity against various other rare clinical samples of microbial species.