Introduction
The COVID-19 pandemic, resulting from the SARS-CoV-2 virus, has affected over 2.8 million people. Individuals and resulted in over 198,000 deaths in 200 countries since it first emerged in Wuhan, China.1 The mortality rate of COVID-19 exhibits significant variation across different countries, ranging from 0.7% in Germany to 10.8% in Italy.2 It is worth noting that older persons and those Individuals with pre-existing medical conditions are more likely to have a less positive outlook. 3 Diabetes mellitus (DM) is now recognized as a serious comorbid condition linked to severe illness, acute respiratory distress syndrome (ARDS), and increased mortality in COVID-19 patients. 4, 5, 6 Within a cohort of 72,314 cases, it was shown that patients with DM in China had a death rate of 7.3%, which is higher than the average mortality rate of 2.3%. 7 DM was found in 20.3% of COVID-19 patients who died in Italy. 8 The new coronavirus illness (COVID-19) has escalated into a worldwide pandemic, impacting more than 200 nations and causing a significant number of deaths. Although the overall death rate is very low,9 DM is increasingly acknowledged as a notable concurrent medical disease linked to severe sickness, acute respiratory distress syndrome (ARDS), and increased mortality in persons with COVID-19. 10 DM is increasingly acknowledged as an autonomous risk factor that may independently predict the likelihood of being referred to the ICU. Ensuring optimal management of blood sugar levels is crucial as it enhances the innate immune system, potentially preventing severe outcomes.
However, the nationwide lockdown implemented by governments to contain the pandemic has led to a decrease in the comprehensive management of diabetes. During the last two years, the pandemic had considerable indirect impacts on healthcare services and enduring repercussions on those who have contracted the virus. Ensuring optimal management of blood sugar levels is crucial, as it enhances the innate immune system and may prevent severe COVID-19 outcomes. However, nationwide lockdowns have disrupted comprehensive diabetes management, impacting healthcare services. Combining effective glucose control with protocols categorizing and treating COVID-19 patients and contacts, could offer a more robust approach. 11 This emphasizes maintaining basic strategies like social distancing and face masks. Integrating blood sugar management with protocols may improve outcomes and mitigate the pandemic’s indirect impacts on healthcare and patients with comorbid conditions. The scientific community has responded to this worldwide epidemic by taking extraordinary measures, such as conducting in vitro experiments, clinical trials, and big-data analytics, to understand the intricate connections between DM and coronavirus disease 2019 (COVID-19).
This study seeks to review the existing corpus of research to investigate three essential questions:
Discussion
Diabetes in COVID
The current evidence does not conclusively indicate that individuals with DM pose an elevated susceptibility to acquiring COVID-19. 12 DM has been recognized as a distinct factor that might forecast catastrophic consequences, such as the hazard ratio for admission to the intensive care unit, requirement for invasive ventilation, or mortality in COVID-19 patients is 1.59, with a 95% confidence range ranging from 1.03 to 2.45. 13 The specific features that distinguish type 1 diabetes mellitus (T1DM) from type 2 diabetes mellitus (T2DM) have not been fully determined. Nevertheless, both forms of diabetes are very likely to be linked with a worse outcome in COVID-19 instances. 14 The relationship between DM and the severe repercussions of COVID-19 may be understood via many pathophysiological pathways. A possible reason for this is a decline in the body's inherent immunological function, the first barrier against SARS-CoV-2. This deficiency is particularly noticeable in individuals with uncontrolled DM. DM is linked to the decreased expression of angiotensin-converting enzyme 2 (ACE2) in several organs, such as the lungs (particularly in type II pneumocytes), kidneys, intestines, and vascular endothelium. Under normal conditions, ACE2 breaks down angiotensin-II and, to a lesser extent, angiotensin-I into smaller peptides called angiotensin (1-7) and angiotensin (1-9), respectively, using enzymes.
The pulmonary ACE2/Ang (1-7) system mitigates inflammation and oxidative damage. ACE2 is well recognized for its capacity to provide defense against severe avian influenza A H5N1 infection. 15 The diminished expression of ACE2 in patients with DM may contribute to their increased vulnerability to severe pulmonary injury and acute respiratory distress syndrome (ARDS) in cases of COVID-19. 16 Given the seriousness of the pandemic and the lack of a definitive cure for COVID-19, individuals with DM need to exercise utmost caution and adhere to all necessary precautions. After undergoing a thorough and demanding process, regularly practicing social distancing and consistently keeping proper hand hygiene is crucial.Moreover, it is essential to emphasize the achievement of optimum glycemic control, as it can enhance the functioning of the innate immune system. 17 Recent research conducted in China revealed that aged individuals diagnosed with type 2 DM showed increased fasting blood glucose levels throughout the COVID-19 epidemic. 18 Telemedicine discussions with healthcare specialists might aid diabetic patients in managing the challenges brought up by lockdowns. 19 While animal studies have shown that some anti-diabetic medications, 20 such as pioglitazone and liraglutide, may enhance the expression of ACE2, no evidence suggests that altering existing prescription regimens is necessary.
Interplay of COVID-19 and DM
Numerous factors contribute to the increased vulnerability of individuals with DM to severe COVID-19. These include enhanced cellular binding affinity, effective individual increased susceptibility to hyperinflammation and cytokine storms due to viral entry, reduced capacity to remove the virus, impaired T cell activity, and an increased likelihood of developing cardiovascular diseases. Studies indicate that individuals with diabetes have decreased phagocytosis by neutrophils, monocytes, and macrophages, which affects the ability of neutrophils to move toward bacteria, kill bacteria, and the immune system's overall function. 21 Even a brief period of high blood sugar levels may weaken their natural immune response. Patients with diabetes also exhibit impaired adaptive immunity. Hyperglycemia, common in diabetes, hampers immune cell function, particularly in macrophages and T cells, reducing pathogen clearance and increasing infection susceptibility, including COVID-19. Diabetes-related immune dysfunction further contributes to the dysregulated inflammatory response seen in severe COVID-19 cases. Chronic hyperglycemia and insulin resistance in diabetes lead to the enhanced synthesis and production of pro-inflammatory cytokines and reactive oxygen species (ROS), developing persistent, mild inflammation and oxidative stress. These factors worsen the inflammatory response to COVID-19, possibly harming tissues and organ-functioning organs. Diabetes is associated with endothelial dysfunction, defined by decreased vasodilation that depends on the endothelium, increased permeability of blood vessels, and a condition that promotes blood clot formation, elevating the risk of thrombosis, a common complication in severe COVID-19. These complexities impart the need for tailored treatment strategies for diabetic COVID-19 patients to enhance outcomes.
Risk factors for COVID-19 by diabetic individuals
Individuals with diabetes may experience poorer outcomes due to various factors, such as elevated hemoglobin levels. Haemoglobin (HbA1c) often weakens immune function, making them more vulnerable to infectious illnesses. 22 COVID-19 causes an increase in blood sugar levels, especially in those who have diabetes, prediabetes, and obesity. 23 For those diagnosed with Type 2 diabetes (T2D) and obesity, marked changes in the initial level of inflammation occur, which causes the activation of white blood cells, increased formation of fibrous tissue, and cell death. It ultimately leads to elevated levels of inflammatory cytokines. DM has shown increased levels of inflammation-related biomarkers, such as Interleukin-6, C-reactive protein, serum ferritin, coagulation index, and D-dimer. It might increase their susceptibility to the cytokine storm in COVID-19 24 infection. Individuals with comorbidities of diabetes and nonalcoholic fatty liver disease, 25 a known risk factor for severe COVID-19, 26 may have an inflammatory response. Hyperglycemia is linked to compromised immune function, increasing the risk of contracting infections and experiencing severe symptoms. 27 COVID-19 virus attaches to the angiotensin-converting enzyme 2 (ACE2) receptor. Subsequently, the quantity of this receptor is diminished. Once the virus enters the body, it causes higher amounts of angiotensin II, damaging cells. 28, 29 Moreover, SARS-CoV-2 has the potential to harm pancreatic ß-cells, which might lead to a reduction in glucose regulation in individuals with preexisting diabetes or even trigger the development of new-onset diabetes, similar to SARS infection.
The COVID-19 pandemic has had a notable influence on persons with diabetes, while no substantiated data indicates elevated infection rates in comparison to the general population. Age, obesity, and other health issues are contributing factors that enhance the likelihood of hospitalization and fatality in this particular population. 30 During a pandemic, there is no evidence or indication of the modification of regular prescription of glucose-lowering therapies. Nevertheless, there has been a noticeable rise in the occurrence of newly developed diabetes and instances of diabetic ketoacidosis. However, the extent to which COVID-19 directly contributes to these patterns remains unknown. Additional investigation is required to examine the enduring consequences of COVID-19, such as the implications of extended COVID-19, alterations in diabetes occurrence after the pandemic, and the immunological response to immunization among individuals with diabetes. There are also concerns regarding possible inequalities in certain communities as a result of vaccination fading and the use of telehealthcare.
Vulnerable populations
Throughout the pandemic, several predictive models for severe COVID-19 outcomes and death have been created, and these models guide making choices on shielding, minimizing, addressing occupational exposure, and prioritizing COVID-19 vaccinations. A new exhaustive research study has identified two promising models undergoing rigorous verification. 31 The first model used the research database in England to analyze data from 8.25 million individuals aged 19–100 years before the onset of the epidemic 32 This model assessed the risk of mortality associated with COVID-19 by considering factors like age, race, socioeconomic status, body mass index (BMI), and many underlying health issues. The assessment revealed exceptional proficiency. An inquiry into the mortality hazards associated with COVID-19 in patients who have both type 1 and type 2 diabetes detected a substantially higher degree adjusted hazard ratios compared to those without diabetes 33 Another study developed a mortality prediction score for COVID-19 patients admitted to hospitals, incorporating variables like age, sex, comorbidities (including diabetes), and various clinical indicators, with high accuracy in predicting mortality risk 34 Research on COVID-19 vaccination outcomes found that while individuals with type 2 diabetes and higher HbA1c levels had increased mortality risks (adjusted HRs), overall mortality rates were lower post-vaccination across all groups. 35
The role of angiotensin-converting enzyme 2 in COVID-19 transmission
While the exact mechanisms behind the enhanced vulnerability of Individuals with diabetes and hypertension who are susceptible to contracting COVID-19 are completely not established, the involvement of ACE2 in the relationship between COVID-19 and diabetes is apparent 36 DM and hypertension are linked to the renin-angiotensin system (RAS) stimulation in many tissues. 37 The RAS system regulates blood volume and systemic vascular resistance. 38 Research has shown that ACE inhibitors and angiotensin II Type-I receptor blockers (ARBs) may enhance the synthesis of ACE2 in the kidneys and cardiovascular system. 39, 40 It might aid in efficiently managing both type 1 and type 2 diabetes. However, the existing evidence that supports the use of ACE/ARBs causes an increase in ACE2 levels in the respiratory system is insufficient. Insufficient evidence exists to indicate if prescribing individuals ACE inhibitors or ARBs to other medications reduces the risk of contracting or experiencing the severity of COVID-19.
Increased ACE2 expression in alveolar AT2 cells and the heart, kidneys, and pancreas in humans 41, 42, 43 has been associated with a more advantageous SARS-CoV-2 binding pattern. Diabetes has elevated levels of ACE2 expression in the lungs, kidneys, heart, and pancreas, 44, 45 which may enhance the susceptibility to SARS-CoV-2 infection. Thiazolidinediones (TZDs) such as pioglitazone, glucagon-like peptide–1 (GLP-1) agonists like liraglutide, statins, and ibuprofen have also been shown to enhance ACE2 expression, 46 which is associated with hypoglycemic effects. Initially, there were concerns about the use of NSAIDs, such as ibuprofen, among persons who have been diagnosed with COVID-19. 47 But World Health Organization (WHO) claimed that there were no substantial adverse effects linked to the use of NSAIDs. Recent research has seen a significant increase in investigations exploring the correlation between diabetes and the manifestation of ACE2 in the human lungs. Rao et al. performed a phenome-wide Mendelian randomization investigation, which indicated that elevated ACE2 expression in the lungs is associated with a greater vulnerability to severe SARS-CoV-2 infection and is causally connected to diabetes. 48
Cytokine storm
Diabetic individuals diagnosed with covid 19 undergo a continuous, mild inflammation due to cytokine storm. 49 They have a compromised adaptive immune system characterized by a delayed Th1 cell-mediated immune response and a subsequent hyperinflammatory reaction. 50 The augmented pro-inflammatory cytokine reaction is characterized by increased levels of cytokines IL-1, IL-6, IL-8, and TNF-a. Advanced glycation end products (AGEs) 51 may partly contribute to this reaction. AGEs are chemical compounds made up of glucose and lysine or arginine residues that accumulate in poorly regulated diabetes and can stimulate cytokine production even in non-diabetic cells, suggesting a role in increased cytokine levels in diabetes. High glucose levels alone lead to increased cytokine production, but upon glucose reduction, cytokine production decreases compared to a glucose-free condition. The reduced interleukin production upon glucose reduction may also result from inherent cellular abnormalities in diabetic patients. 52 Diabetes-related chronic inflammation is further exacerbated by SARS-CoV-2 infection, leading to an increased inflammatory response. Studies using a mouse model for MERS-CoV infection, designed to resemble human characteristics, demonstrated that male mice with diabetes suffered a more severe and extended sickness. This was evident via changes in the number of CD4+ T cells and abnormal cytokine reactions. 53 Research on diabetic and COVID-19 patients has shown a change in the quantity of CD4+ and CD8+ T lymphocytes in the peripheral area, along with increased cytokine levels.
AMPK/mTOR signaling pathway
Significant research highlights AMPK signaling dysfunction in individuals with metabolic syndrome and DM. 54, 55, 56 Activating AMPK may enhance insulin sensitivity by increasing glucose transportation and absorption and boosting fatty acid oxidation. 57 Metformin, an AMPK activator discovered in 2001, is currently used to treat type 1 and 2 diabetes. 58 AMPK inhibits the mTOR pathway, which is more active in DM due to reduced AMPK function. Metformin is thought to influence AMPK and mTOR regulation. Metformin enhances beta cell activity and the efficacy of influenza vaccinations in individuals diagnosed with type 2 diabetes and obesity. 59 AMPK is a vital energy sensor inside cells, regulated by glucose levels. The signaling pathway of this system is critical for managing cellular energy homeostasis by modulating several biological processes, including metabolism, growth, and proliferation. The mTOR pathway, regulated by AMPK, is influenced by one of the primary pathways of either mTOR complex 1 (mTORC1) 60, 61, 62 or mTOR complex 2 (mTORC2), which has distinct protein partners. The mTORC1 complex, composed of mTOR, mLST8, and raptor, regulates protein synthesis and cell size via activation of p70S6 kinase (p70S6K)/S6 kinase 1 (S6K1) and 4E-binding protein 1 (4E-BP1).
Conversely, mTORC2, composed of mTOR, mSIN1, mLST8, and Rictor, controls cell survival and cytoskeleton arrangement by phosphorylating protein kinase B (PKB/Akt) at serine 473. AMPK is activated in response to a reduction in cellular energy levels. 63 This stimulation leads to an increase in glucose uptake in skeletal muscles, enhancement in fatty acid oxidation in adipose tissues, and a decrease in the synthesis of glucose in the liver.
Impact of diabetes medications
Most guidelines recommend tight glycemic control, increased continuous monitoring, and implementation of supportive treatments essential in mitigating diabetic ketoacidosis (DKA). 64, 65, 66 Exercise caution while utilizing SGLT2 inhibitors is being implemented because of the possible hazards of ketoacidosis. Empirical investigations conducted to observe and analyze phenomena in their natural settings consistently demonstrate a positive correlation between the use of metformin and improved results. In contrast, the use of insulin is related to negative outcomes in hospitalized persons. An extensive review of 18 studies, which included a total of 12,277 individuals diagnosed with both diabetes and COVID-19, revealed a strong and significant link between the usage of insulin and a higher likelihood of death. 67 Surprisingly, the administration of insulin as a remedy is related to an increased chance of hospital admission in individuals with type 2 diabetes; the odds ratio (OR) was 1.31 with a 95% confidence interval (CI) of 1.06 to 1.61. Nevertheless, those diagnosed with type 1 diabetes and who received insulin therapy saw a significant decrease in the likelihood of being admitted to the hospital (odds ratio 0.14; 95% confidence interval, 0.05, 0.35). 68
It is essential to recognize that these conclusions are based on restricted research. Observational studies are prone to many biases related to individual behaviors, characteristics, and the healthy user effect. Randomized controlled trials (RCTs) are the most dependable approach for assessing the effectiveness of interventions, including pharmacological treatments. Only a few RCTs have assessed the effectiveness of glucose-lowering treatments in COVID-19 individuals with diabetes. The dapagliflozin in respiratory failure in individuals with COVID-19 (DARE-19) experiment is a significant investigation that included 1250 individuals hospitalized with COVID-19 and had at least one cardiovascular risk factor. 69, 70 The trial used a double-masked, placebo-controlled design and showed that dapagliflozin was well tolerated and seemed to reduce instances of organ failure. The study could not demonstrate the statistical significance of its main goals, which were to avoid the occurrence or progression of organ dysfunction or mortality, as well as the combined outcome of recovery during 30 days.
Glucose lowering therapies in viral infection
Several hypoglycemic medications demonstrate additional effects beyond glucose reduction that may aid in the prevention of severe COVID-19 consequences. These medications can reduce biochemical levels that cause inflammation, correct anomalies in blood clotting, and regulate the expression of ACE2, all of which contribute to treating COVID-19. An innovative and comprehensive analysis thoroughly examines the anti-inflammatory characteristics of certain glucose-lowering medications. 71 Moreover, several medicines can potentially have protective effects on the primary organ systems often impacted by SARS-CoV-2. Metformin, a frequently prescribed medication for obese diabetic individuals, has potential advantages for cardiovascular health and does not cause low blood sugar levels. Biguanides, including metformin, effectively manage several viral illnesses, including H3N2 influenza, hepatitis C, hepatitis B, and HIV. 72 Research conducted on people with type 2 diabetes found that those undergoing biguanide medication had a reduced occurrence of H3N2 influenza infections compared to those using insulin and sulfonylureas. 73 DPP-IV inhibitors have shown favorable effects on inflammatory and coagulation pathways, which may reduce the likelihood of negative outcomes in COVID-19. Research suggests that initiating dipeptidyl peptidase-IV inhibitors leads to a decrease in the production of cytokines, namely IL-6, IL-8, and TNF-α.
Furthermore, sitagliptin, a DPP-IV inhibitor, has been linked to reduced platelet aggregation in individuals diagnosed with type 2 diabetes. 74 Inhibiting DPP-IV/CD26 receptors may decrease the virus's ability to enter and reproduce in the respiratory system, alleviating lung inflammation. People diagnosed with T2DM may have various health issues, such as renal and heart illnesses, due to the COVID-19 virus. The implications are believed to result from the robust inflammatory response the infection elicits. Individuals diagnosed with T2DM who were administered glucagon-like peptide-1 receptor agonists (GLP-1 RAs) showed reductions in interleukin-6 (IL-6) levels and circulating markers of cellular damage. These chemicals have shown the ability to retard the process of platelet aggregation in human in vitro cells. 75 Studies on mice models of induced lung injury have also shown the benefits of GLP-1 RAs. 76
These investigations have shown a decline in cytokine levels, alleviated lung inflammation, and preserved lung function after the viral damage. In addition to its hypoglycemic effects, insulin does not directly improve the underlying mechanisms of COVID-19-related issues. Two studies investigating the use of insulin in COVID-19 patients who were hospitalized yielded conflicting results. A study discovered an association between the use of insulin and adverse outcomes, such as prolonged hospital stays and elevated in-hospital mortality rates. 77 Conversely, another study found that those who use insulin had a reduced probability of encountering severe illness, defined as being hospitalized in the critical care unit, needing mechanical ventilation, or leading to death. However, the credibility of these investigations could have been improved by their nonrandomized design and limited sample sizes, which challenges the ability to conclusively determine whether the observed effects were solely caused by insulin or influenced by other patient-related characteristics or confounding variables. Glucose-lowering therapies, including insulin and metformin, have shown potential in managing blood sugar levels during viral infections such as COVID-19. Elevated glucose levels can exacerbate viral replication and inflammation, complicating patient outcomes. Hence, effective glucose control may mitigate these effects and improve recovery. Traditional therapies like camphor vapor and Mandl’s paint have also been employed to relieve symptoms of respiratory infections. Camphor vapor, known for its decongestant properties, helps ease breathing difficulties, while Mandl’s paint, a throat application containing iodine, can alleviate sore throat symptoms. Combining modern and traditional treatments might offer a comprehensive approach to managing viral infections and their complications. 78
Tocilizumab
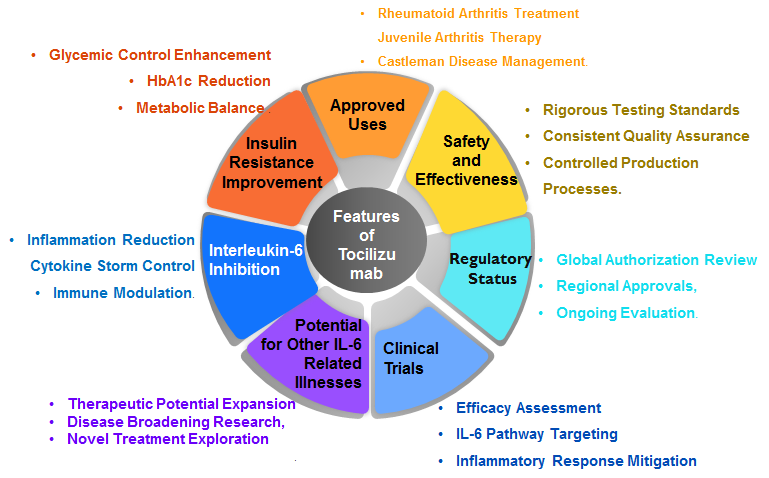
Hydroxychloroquine could be a useful additional medication during the current outbreak of covid 19 for patients with poorly controlled glucose levels. It is affordable, widely available, has a moderate effect in reducing HbA1c, can be taken once a day, and is generally well tolerated. However, it should not be used if the patient has contraindications such as diabetic retinopathy or cardiomyopathy. Tocilizumab is underway in clinical trials to explore the possible use of specifically binding to interleukin-6 (IL-6) in individuals suffering from COVID-19. It has shown enhancements in insulin resistance and reductions in HbA1c levels in persons with rheumatoid arthritis and diabetes mellitus. 79 Tocilizumab (TCZ) is an artificial antibody that binds to the human body's interleukin-6 receptor (IL-6R). Its main use is treating rheumatoid arthritis, systemic juvenile idiopathic arthritis (sJIA), and polyarticular juvenile idiopathic arthritis (pJIA). The safety and effectiveness of tocilizumab in humans are ensured by examining its development, production, and testing methods. Due to the inherent complexity of tocilizumab, achieving exact reproduction is not feasible. Therefore, rigorous process controls are implemented to guarantee uniformity in purity, amount, potency, and identification across several batches. Tocilizumab has been authorized to treat Castleman disease and several forms of arthritis in Japan. 80 In the European union, it has been authorized specifically for moderate-to-severe rheumatoid arthritis. The US Food and Drug Administration released authorization for DM in covid illness in the United States. Tocilizumab has also been investigated for its potential efficacy in treating other illnesses associated with IL-6, such as Crohn's disease 81 (Figure 1).
Comparison of COVID-19 outcomes in individuals with type 1 and type 2 diabetes
A new prospective cohort study done at Vanderbilt University Medical Center found that both Type 1 (T1D) and Type 2 diabetes (T2D) have a higher likelihood of hospitalization and more severe disease compared to those without diabetes. 82 Research conducted in England revealed that individuals diagnosed with both Type 1 (T1D) and Type 2 Diabetes (T2D) had an elevated likelihood of mortality from COVID-19 during hospitalization, even after accounting for demographic variables. 83 A study conducted in France showed that those identified with Type 1 diabetes (T1D) had a reduced likelihood of experiencing a terrible outcome compared to those diagnosed with Type 2 diabetes (T2D). 84 Collectively, these studies demonstrated the relationship between Type 1 Diabetes (T1D) and Type 2 Diabetes (T2D) are different from one another in terms of variables that increase the likelihood of experiencing more severe symptoms of COVID-19. The odds ratios and confidence intervals provided in these studies further emphasize the extent of these risks. The study from Vanderbilt highlighted the importance of early intervention and continuous monitoring for diabetic patients during the pandemic, stressing that timely medical care can significantly reduce the risks of severe outcomes. The French research also suggested potential differences in the biological mechanisms underlying T1D and T2D that might influence COVID-19 severity, proposing a need for tailored treatment strategies. Furthermore, demographic factors such as age, gender, and comorbidities played a crucial role in the severity of COVID-19 among diabetic patients, underscoring the importance of personalized medical approaches in managing these patients during the pandemic.
Guidelines for the care of individuals with diabetes during the global pandemic
International guidelines for managing the COVID-19 epidemic exacerbate the impact of stress on individuals with diabetes, emphasizing the critical need for optimal glycemic control and overall health to lower the risk of severe illness. 85 These guidelines advise regular blood glucose monitoring, adherence to medication regimens, and the maintenance of a healthy lifestyle, incorporating a balanced diet and regular exercise. A balanced diet rich in essential nutrients is crucial in maintaining health during the COVID-19 pandemic. During the pandemic, prioritizing nutrition helps strengthen immunity, manage stress, and improve recovery outcomes, emphasizing the importance of a well-rounded diet in these challenging times. 86 Telemedicine consultations are encouraged to limit virus exposure, ensuring continuous medical support while reducing the risk of infection. Patients are advised to maintain an ample supply of medications and necessary supplies to avoid disruptions in their diabetes management. Special attention is given to older adults who require tailored care due to their higher susceptibility to severe COVID-19 outcomes. Mental health support is also essential, given the pandemic's profound impact on stress levels, which can negatively affect glucose control. These guidelines offer comprehensive, evidence-based strategies for effectively managing diabetes during the pandemic, enhancing health outcomes, and reducing the risk of complications. They also underscore the importance of a multidisciplinary approach involving healthcare providers, caregivers, and patients to ensure holistic care and support during these challenging times. By fostering a collaborative environment and leveraging technology, these guidelines strive to mitigate the pandemic's impact on individuals with diabetes, promoting resilience and long-term health.
Tele health for diabetes patients in COVID-19
Given the increased vulnerability of individuals with diabetes to severe cases of COVID-19, it is critical to inform patients about the vital significance of maintaining optimum metabolic and glycemic management. It is vital to address the COVID-19 symptoms that may discourage patients, especially those with uncontrolled blood glucose levels, from seeking medical help for diabetes. Telehealth services have become a viable means of delivering continuous medical treatment while reducing the risk of COVID-19 exposure. Studies on telemedicine in diabetes treatment have shown encouraging results, showcasing its efficacy in providing healthcare, providing guidance on lifestyle changes, and enabling self-monitoring of important health markers, 87 including blood glucose and blood pressure. Telemedicine has also been discovered to reduce HbA1c levels 88 effectively. An analysis of a US claims database uncovered a striking surge in the adoption of telehealth services by a factor of 100 from 2019 (0.3%) to 2020 (29.1%). The study observed that the increase in telemedicine did not have a detrimental effect on prescription filling or glycemic control. 89 Online medication delivery systems have proved effective in mitigating COVID-19 exposure, as evidenced by many studies in China. 90, 91 When deciding between in-person visits and telemedicine consultations, it is important to consider the local COVID-19 infection rates and individual patient characteristics.
Cumulative risk is an important factor to take into account. For instance, having five in-person appointments may have a higher risk than having one in-person visit followed by four telemedicine exams. If patients encounter telemedicine difficulties, an in-person examination may be more appropriate. Optimizing antihyperglycemic medication is critical for attaining HbA1c objectives. However, caution should be used when considering the early discontinuation of established therapy. During the pandemic, prompt treatment escalation to injectable medication may need telemedicine. Research has shown that telehealth monitoring can improve assistance for individuals diagnosed with type 2 diabetes who are beginning insulin therapy. This medication has been shown to successfully decrease HbA1c levels in individuals diagnosed with type 1 diabetes who use an insulin pump, even without in-person visits for six months, without an increase in diabetic ketoacidosis. 92
Recovery from the COVID pandemic
In the inpatient setting, the deterioration of glycemic control in hospitalized individuals may stem from acute or chronic inflammation and aggravates insulin resistance and high blood sugar levels. To effectively manage patients admitted to the hospital, it is important to have a team of experts from different disciplines who specialize in diabetes care. It includes advanced technology like continuous glucose monitoring to monitor blood sugar levels, achieving the best possible control of blood sugar levels, providing treatments for COVID-19 that are supported by scientific evidence, educating patients about their condition, and ensuring their overall well-being healthcare professionals. 93, 94, 95 Given the increased risks for patients recovering from SARS-CoV-2 infection, early post-discharge follow-up is essential to reduce the risk of death or readmission. Previous instances of natural disasters in community settings have shown that temporary interruptions in healthcare may result in adverse consequences for persons with diabetes. These consequences include inadequate management of crucial risk variables such as glycemic control, blood pressure, and cholesterol levels, and a decline in emotional well-being.
Furthermore, these interruptions have a detrimental influence on the general well-being of individuals and the economic state of affairs. The whole ramifications of the COVID-19 pandemic's effect on individuals with diabetes for two years is yet to be seen; it is expected to be more severe than the direct effects of COVID-19. As healthcare systems move into the recovery phase, it is crucial to prioritize early assessment and care processes for individuals with diabetes, including face-to-face consultations. The pandemic has accelerated the adoption of remote consultations (e.g., telephone, video, and e-consultations). Still, it's important to address potential inequalities in access, particularly among deprived populations, older adults, and ethnic minorities, to avoid exacerbating disparities seen during the pandemic.
Conclusion
The COVID-19 pandemic has underscored the heightened vulnerability of individuals with diabetes mellitus (DM) to severe outcomes, including acute respiratory distress syndrome (ARDS) and increased mortality. The intricate interplay between DM and COVID-19 is mediated through several pathophysiological mechanisms, notably impaired immune function and decreased ACE2 expression. Optimal glycemic control is critical for enhancing the immune response and mitigating severe complications. The pandemic has disrupted diabetes management, emphasizing the need for innovative approaches like telemedicine. Medications such as hydroxychloroquine and tocilizumab are being explored for their potential benefits in managing both diabetes and COVID-19 symptoms. International guidelines stress the importance of regular monitoring, medication adherence, and lifestyle modifications to improve overall health and reduce severe illness risk. These comprehensive strategies aim to support diabetic patients through the pandemic, fostering resilience and better health outcomes.