- Visibility 101 Views
- Downloads 25 Downloads
- Permissions
- DOI 10.18231/j.ijmmtd.2020.030
-
CrossMark
- Citation
Intestinal Parasitic infestations in children visiting Pravara Rural Hospital, Loni (Maharashtra-India)
- Author Details:
-
Shahriar B Roushani
-
Anagha Kinikar
-
Deepika Bhalerao
-
Savita Tajane *
Abstract
Background: Intestinal parasitic infections represent major health problem particularly in tropical countries. Intestinal parasitic infections are closely related to poor sanitation and socioeconomic status. In rural populations these infections are common as most of population belong to low socioeconomic group and also lack proper hygiene. These infestations has implications for child health in terms of physical growth retardation and development.
Materials and Methods: This two years prospective study was carried out in Dept. of Microbiology, Rural medical college, (PIMS-DU) Loni. All stool specimens from children (0 -14 years) received in Dept. of Microbiology were included in the study. All stool specimens were subjected to macroscopic and microscopic examination. Both saline wet mount and iodine wet mount were prepared and examined for microscopic features.
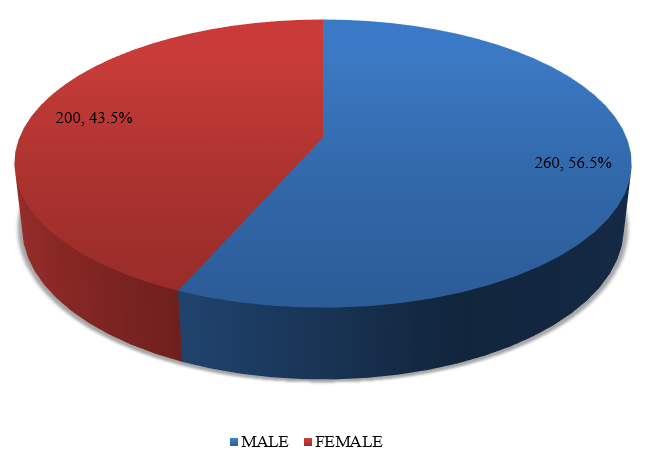
Results: A total of 460 stool specimens were received during the study period. Males (56.5%) outnumbered females (43.5%) in the present study. Maximum children belonged to age group 1 - 5yrs. A total of seven stool specimen showed parasites giving the positivity 1.52%. Commonest intestinal parasite was found to be E. histolytica in our study. We found one case of H. dimunita which is quite uncommon parasite.
Conclusions: Intestinal parasitic infestations like amoebiasis, hookworm, ascariasis exertdiverse clinical manifestation such as malnutrition, iron deficiency anemia, intestinal obstruction. Presence of parasitic infections is expected to be high in agricultural rural population. But we found the quite low positivity in our area may be owing to better sanitation awareness and compliance to Government deworming health program.
Introduction
Intestinal parasitic infestations are among the most common infestations around the world wide. It is distributed with high prevalence in poor and socio-economically deprived communities in the tropics and subtropics. These infestations are one of the global health problem, particularly among the children in poor communities in developing countries.[1]
Parasitic infections involving gastro intestinal system are caused by protozoa and helminths. The prevalence of parasitic infections varies with the level of sanitation. The impure drinking water, low socioeconomic state, low health status and lack of personal hygiene provide optimal conditions for the growth and transmission of intestinal parasites. Worms infestation is one of the major causes of childhood malnutrition, anemia, stunted physical growth and psycho social problems. Majority of intestinal parasitic infections occur through ingestion of food contaminated with eggs. Protozoal infection occurs through ingestion of encysted stage. Faecal contamination of drinking water, vegetables and food with these cysts is the source of infection. [1], [2]
Some of the helminthic infections are seen when man walks bare foot on faecally contaminated soil. Mode of infection for hookworm infection is the penetration by filariform larvae through the skin in human being.[3] Also cercarial forms of certain Schistosoma species may penetrate the skin of person coming in contact with water. Autoinfection in children, owing to their habit of scratching perianal area and put the fingers in mouth is known in E. vermicularis parasite.[4]
Role of carriers and fomites cannot be ignored in transmitting these infections. A carrier can be healthy or convalescent. Houseflies may transmit the egg /cyst from faeces to unprotected food. In country like India where, there are minimal sanitation measures or hygiene is not up to the mark, parasitic infections are commonly seen. Many researchers have studied the prevalence of parasitic infections in different parts of India.[5], [6]
Majority of the parasitic infections are asymptomatic. But some intestinal parasite may present with abdominal pain, diarrhoea, dysentery, steatorrhoea, constipation. Usually, hepatic complications are seen after 1-3 months of dysentery attack in E. histolytica infection. Mechanical effects of roundworm may lead to intestinal obstruction, intussception, and perforation. Occasionally, parasite affects visceral organs like liver, lung and brain as in some tapeworm infections.[7]
Although, global public health problem, parasitic infestation have largely been overlooked by clinicians. But clinical severity and complications by worm infestations are not uncommon. Early diagnosis and institution of appropriate therapy is possible to control parasitic infestation in community.
Most of the parasitic diseases cannot be conclusively diagnosed only on the basis of clinical features and physical examination. These require the support of the laboratory to firmly establish the diagnosis. Various laboratory methods are available to diagnose parasitic diseases. Direct demonstration of adult parasites /segments /larvae in stool specimen / tissue is easy but not always practicable. Microscopic examination of stool specimen, body fluids and tissues is standard method followed. Extended methods like culture, xenodiagnosis, animal inoculation and immune-diagnosis are also existed. Radiological examination, radioisotope study, ultrasound (USG), magnetic resonance imaging (MRI) are imaging techniques to localize the suspected infection. Intradermal test based on immediate hypersensitivity are available for parasite like E. histolytica and E. granulosus.[7]
The aim of the study was to know the presence of intestinal parasites in children <14 years in and around our rural institute set up.
Material and Methods
This two years prospective study was carried out in the Department of Microbiology, Rural Medical College, Loni (PIMS-DU 413 736) Maharashtra(India). A total of 460 stool specimens were received from various OPD and IPD departments during study period.
Collection of specimen
All stool specimens were collected in a sterile, clean wide mouthed well labeled container after giving proper instructions to avoid contamination with water, urine, or disinfectants. Due care was taken to transport the specimen without delay and examination as early as possible.
Macroscopic examination
Stool specimen was examined for its consistency, color, odour, presence of blood or mucus, worms or segments.
Microscopic Examination
On glass slide, a small amount of stool sample was emulsified in 1-2 drops of saline and iodine wet mount. A cover slip was placed on it, with care that preparation was free of air bubbles and macroscopic debris. Wet mount preparations were observed first under low (10X) and then high (40X) objectives. [7], [8]
Observations and Result
| Age (Years ) | Male | Female | Total | Percentage (%) |
| <1 | 87 | 56 | 143 | 31.1% |
| 1- 5 | 104 | 79 | 183 | 39.78 % |
| >5-12 | 63 | 60 | 123 | 26.73 % |
| 12-14 | 06 | 05 | 11 | 1.30 % |
| Total | 260 | 200 | 460 | - |
| Total stool specimens | Parasite positivity (%) |
| 460 | 7 (1.52%) |
| Age group ( years ) | 1 to <5 | 5-12 | >12-14 | Total | Percentage | |||
| Gender | M | F | M | F | M | F | ||
| E. histolytica | 01 | -- | 01 | 01 | -- | -- | 03 | 42.85 % |
| Hookworm | 01 | -- | 01 | -- | -- | -- | 02 | 28.57% |
| H. nana | -- | -- | -- | 01 | -- | -- | 01 | 14.28% |
| H. diminuta | -- | -- | -- | 01 | -- | -- | 01 | 14.28 % |
Result
The present study revealed, higher male study population (56.5%) than females (43.5%) ([Figure 1]). Study population showed maximum number of specimens from 1-5 years age group (39.7%) followed by 0 -1 year age group (31.1%).([Table 1]). Out of 460 specimens only 7 specimen showed parasite. Microscopic positivity of stool specimens, was found to be 1.52 %.([Table 2]). Commonest intestinal parasite was found to be E. histolytica (42.8%) ([Table 3]).
Discussion
This two years prospective study was carried out on 460 patients attending the OPD and /or admitted in the hospital due to diarrhoea, weight loss, abdominal pain, vomiting and whose sample were received in the Department of Microbiology, Rural medical college, (PIMS-DU) Loni - 413 736. All stool specimens from children (0 -14 years) were received in wide mouth sterile container. All the stool specimens were subjected to macroscopic and microscopic examination. Macroscopic examination included the colour, consistency, and odour, presence of blood and mucus and nature of the stool specimen. Microscopic examination included preparation of saline and iodine wet mount.
In the present study, we observed higher male population (56.5%) than females (43.5%) which is quite similar to studies done by Saurabh et al. and Dhruba et al. who reported males as (57.8%) and (64%) respectively.[2], [9] In contrast Chang et al. reported female population at higher side stating that gastrointestinal disorders were more commoner in females.[10]
We included all children <14 years in the present study. Maximum number of the samples were from age group (1-5year group) followed by less than one year age. We received very less number of samples between 12-14 age group possible age of hesitancy. Study by Dambhare et al. included only school going children (6-14 years) population. [11] Some researcher’s also included infants and toddlers.[1], [9] Our study population, contained 143 stool specimens from infants but all were negative for parasite, indicating very less chances of infants being infected.
A Total of 7 stool specimens showed parasites giving parasite positivity as 1.52% in the present study. Positivity of stool samples found to be quite low in our rural area as against the presence of parasitic infections is expected to be high in agricultural rural population. The positivity may be low as larger portion of children visiting Pravara Rural Hospital are investigated by clinicians to rule out parasitic infection though patient may not have any related symptoms. A study by Dambhare D G,et al in Wardha, found it to be as 7.56%.[11] While Shanker Venkatesh et al from Adilabad reported the more positivity (66%) by formalin ether sedimentation technique than saline wet mount (36%) in their tribal study. [12] Similarly Rajvir singh et al., Beena Jad et al, and Ravish kumar et.al reported positivity as 6.68%, 7.8%, and 8.12% respectively.[13], [14], [15]
Highest parasitic infection is reported by Sucheta et al, Dhruba et al. and Rashid et al. as 42.14%, 31.2%, and 22.3% respectively.[16], [9], [17] Maximum positivity in these studies may be due to presence of symptomatic cases in larger number in their study population.
In our study the commonest intestinal parasite was found to be cyst form of E. histolytica (42.8%) followed by eggs of Hookworm (28.5%) and H. nana (14.2%). Our findings was comparable to Dhruba et al who reported E. histolytica as 38.4%. [9] Similarly, study by Shakya et al. reported prevalence of E. histolytica as 8.01% and Choubisa et al. as 8.92%.[18], [19]
Most of the studies revealed the E. histolytica as commonest intestinal parasite. [20], [1], [21]
Whereas Rajender Singh et.al from Dehradun in their study reported, Giardia lamblia as most common intestinal parasite and Ravish Kumar et al. reported it as second most. [5] Proportionately, helminths were dominated in most of the studies in India. [9], [2] We could catch one case of Hymenolepis diminuta in our study. H. dimunita is not frequently seen as H. nana infection. H. dimunita require an intermediate host for it’s transmission in humans. [22] Sometimes this parasite may present with convulsions and asthma as reported by Sethi et al.[23] In the present study the child was presented with fever, dry cough and vomiting.
Positivity was maximum in age group (5-12 years) which is likely age of outdoor playing especially in farms in rural locality. The age group 12-14 showed no parasite may be due to adoptions of hygienic methods in this early adolescent group. The present study revealed, slightly higher positivity in males (57.1) which is similar to Sourabh et al. from their Ambajogai study.[2] In contrast Shakya et al. and Tamirat et al. reported more parasite positivity in females, in their respective studies.[18], [24]
In our study, positivity of stool samples found to be quite low compared (1.52%) to other similar studies in India. Overall male preponderance of study population shows high seeking behaviour among males of health facilities. Low positivity of intestinal parasites in children might be due to improved sanitation and personal hygiene as a result of various awareness programme by our medical college and hospital in surrounding areas. In addition it may to be due to effective deworming programme by health authorities in our area.
Conclusion
Stool examination is still a gold standard test for screening of intestinal parasitic infections in community. Presence of these infections varies with different geographic locations and level of sanitation. Present study focussed the presence of intestinal parasitic infection among children in our rural region. Study outcome revealed lesser number of intestinal parasitic infestations in our agricultural led rural population as a result of an effective integrated approach of health care services.
Source of Funding
None.
Conflict of Interest
None.
References
- Shobha M, Bithika D, Bhavesh S. The prevalence of intestinal parasitic infections in the urban slums of a city in Western India. J Infect Public Health. 2013;6(2):142-9. [Google Scholar]
- Chakraborty S, Nilekar SL. Prevalence of Intestinal Parasitic Infestations in and Around Ambajogai, Maharashtra. Int J Curr Microbiol App Sci. 2019;8(03):406-14. [Google Scholar]
- Agrawal PK, Rai SK, Lk K, Ghimire G, Banjara MR, Singh A. Intestinal Parasitic infection among patients attending Nepal Medical College Teaching Hospital. Nepal Med Coll J. 2012;14(2):80-3. [Google Scholar]
- Ragunathan L, Kalivaradhan SK, Ramadass S, Nagaraj M, Ramesh K. Helminthic Infections in School Children in Puducherry, South India. J Microbiol, Immunol Infect. 2010;43(3):228-32. [Google Scholar]
- Singh R, Aggarwal RK, Koul N. Prevalence of Intestinal Parasites at a Tertiary Care Centre at Dehradun, Uttarakhand, India. Int J Curr Microbiol App Sci. 2019;8(06):932-7. [Google Scholar]
- Hedge GR. Prevalence of intestinal parasitic infestation in rural area. J Postgr Med. 1986;32:225-8. [Google Scholar]
- Chatterjee KD. ParasitoIogy (protozoology and helminthology) in relation to clinical medicine. . 2009. [Google Scholar]
- Collee JG, Fraser AG, Marmion BP, Simmons A. Simmons. Mackie & McCartney Practical Medical Microbiology. . 2006. [Google Scholar]
- Chandi DH, Lakhani SJ. Prevalence of Parasitic Infections among School Children in Bhaili, Durg, Chhattisgarh. Int J Curr Microbiol App Sci. 2018;7(09):1919-25. [Google Scholar]
- Chang L, Toner BB, Fukudo S, EG, GRL, Norton NJ. Age, Society, Culture, and the Patient's Perspective in the Functional Gastrointestinal Disorders. Gastroenterol. 2006;130(5):1435-46. [Google Scholar]
- Dambhare DG, Bharambe MS, Garg B. Intestinal Parasites Prevalence and Related Factors among School Children in the Rural Area of Central India. J Commun Dis. 2010;42(4):281-6. [Google Scholar]
- Shanker BM, Venkatesh S, Rao N, Vivekanand, Bmsv. AComparative Study of Concentration Techniques for Detection of Intestinal Parasitic Infections to Evaluate the Prevalence and to Identify A Better Method of Concentration Technique At A Tribal Tertiary Care Hospital. IOSR J Dent Med Sci. 2016;15(7):42-6. [Google Scholar]
- Singh R, Singla P, Sharma M, A. Prevalence of Intestinal Parasitic Infections in a Tertiary Care Hospital in Northern India: Five year retrospective study. Int J Curr Microbiol App Sci. 2013;2(10):112-7. [Google Scholar]
- Jad B, Raina S, Grover P. Prevalence of intestinal parasites among patients of a tertiary hospital in Ambala city, Haryana, India. Int J Res Med Sci. 2015;3(12):3753-8. [Google Scholar]
- Kumar M, Doddamani PK, Parandekar P, Kumar P. Prevalence of Intestinal Parasitic Infections at a Tertiary Care Hospital: a Retrospective Study. Int J Curr Microbiol App . 2019;8(06):2822-7. [Google Scholar]
- Lakhani SJ, Khara RR, Joshi S, Vasisht S. Intestinal Parasitic Infestations Among School Children in Piparia Village, Vadodara District. Int J Scientific Res. 2012;2(12):434-6. [Google Scholar]
- Rashid MK, Joshi M, Joshi HS, Fatemi K. Prevalence of Intestinal Parasites among School Going Children In Bareilly District. National J Integr Res Med. 2011;2(1). [Google Scholar]
- Shakya B, Shrestha S, Madhikarmi NL, Adhikari R. Intestinal Parasitic Infection among School Children. J Nepal Health Res Counc. 2012;10:20-3. [Google Scholar]
- Choubisa SL, Jaroli VJ, Choubisa P, Mogra N. Intestinal parasitic infection in Bhil tribe of Rajasthan, India. J Parasit Dis. 2012;36(2):143-8. [Google Scholar]
- Langbang D, Dhodapkar R, Parija CS, Premarajan KC, NRK. and Nonika Rajkumari Prevalence of intestinal Parasites among rural and urban population in Puducherry ,South India-A Community -based study. J Family Med Prim Care. 2019;8(5):1607-12. [Google Scholar]
- Gelaw A, Anagaw B, Nigussie B, Silesh B, Yirga A, Alem M. Prevalence of intestinal parasitic infections and risk factors among schoolchildren at the University of Gondar Community School, Northwest Ethiopia: a cross-sectional study. BMC Public Health. 2013;13(1):304-14. [Google Scholar]
- Parija SC, Cestodes. Cestodes: Cyclophyllidean tapeworms. . 2013. [Google Scholar]
- Khurana S, Sethi S, Gupta S, Jayshree M, Mewara A. Hymenolepis diminuta infection in a child from urban area of North India: A rare case report. Trop Parasitol. 2018;8(2):118-200. [Google Scholar]
- Hailegebriel T. Prevalence of intestinal parasitic infections and associated risk factors among students at Dona Berber primary school, Bahir Dar, Ethiopia. BMC Infectious Diseases. 2017;17. [Google Scholar]
How to Cite This Article
Vancouver
Roushani SB, Kinikar A, Bhalerao D, Tajane S. Intestinal Parasitic infestations in children visiting Pravara Rural Hospital, Loni (Maharashtra-India) [Internet]. IP Int J Med Microbiol Trop Dis. 2020 [cited 2025 Oct 15];6(3):135-138. Available from: https://doi.org/10.18231/j.ijmmtd.2020.030
APA
Roushani, S. B., Kinikar, A., Bhalerao, D., Tajane, S. (2020). Intestinal Parasitic infestations in children visiting Pravara Rural Hospital, Loni (Maharashtra-India). IP Int J Med Microbiol Trop Dis, 6(3), 135-138. https://doi.org/10.18231/j.ijmmtd.2020.030
MLA
Roushani, Shahriar B, Kinikar, Anagha, Bhalerao, Deepika, Tajane, Savita. "Intestinal Parasitic infestations in children visiting Pravara Rural Hospital, Loni (Maharashtra-India)." IP Int J Med Microbiol Trop Dis, vol. 6, no. 3, 2020, pp. 135-138. https://doi.org/10.18231/j.ijmmtd.2020.030
Chicago
Roushani, S. B., Kinikar, A., Bhalerao, D., Tajane, S.. "Intestinal Parasitic infestations in children visiting Pravara Rural Hospital, Loni (Maharashtra-India)." IP Int J Med Microbiol Trop Dis 6, no. 3 (2020): 135-138. https://doi.org/10.18231/j.ijmmtd.2020.030
